Excellent summary of the early 2014 state of play in health policy replete with solid historical perspective from Anne-marie and Jim Gillespie.
http://www.smh.com.au/federal-politics/political-news/is-this-the-end-of-medicare-20140609-39t2b.html
Victorian Aboriginal Health Service chief executive Jason King, clinical program manager Andrew Baker and medical director Mary Belfrage. Photo: Eddie Jim
Medicare was always a dogfight. It became law in the most extraordinary circumstances: one of a handful of bills passed during the only joint sitting of Federal Parliament in the nation’s history, after the double dissolution election in 1974.
As the Whitlam government prepared to introduce the system – then known as Medibank – its opponents rallied. The Australian Medical Association marshalled a million-dollar ”Freedom Fund”, donated by members. Determined to stop bureaucrats interfering with patients, it hired a former Miss Australia to front its publicity campaign. The General Practitioners’ Society of Australia circulated a poster depicting social security minister Bill Hayden dressed in Nazi uniform.
Dr Anne-marie Boxall, co-author of Making Medicare, says Whitlam had little support, even from within the Labor Party. The party platform advocated a fully nationalised model, along the lines of the British National Health System. By contrast, Whitlam’s plan was for a public insurance scheme. Health services would be delivered by a mix of public and private providers, paid for by taxpayers and guaranteed for everyone.
”The crucial members of his caucus didn’t agree with him, but he was adamant,” she says. ”He’d done a lot of thinking about it. So he waged the war of public opinion and he won. It’s an amazing political story.”
Medibank began full operation on October 1, 1975, just six weeks before the dismissal of the Whitlam government. The Fraser government tinkered with the system several times before abolishing it – only for it to be revived by the Hawke government in 1984 in almost exactly the same form.
Thirty years later, Medicare enjoys overwhelming public support. Politicians will swear to defend its honour, no matter their stripes or the system’s shortcomings. And yet, in the wake of the federal budget, many people believe Medicare is under threat. The target of most ire is the proposed co-payment for doctor visits, under which even the poorest will have to pay for up to ten appointments each year.
Are these changes the beginning of the end of universal coverage? Or another nail in its coffin? Or are they actually a distraction from the deeper afflictions at the heart of Australia’s healthcare system?
Health Minister Peter Dutton describes the Coalition as ”the greatest friend Medicare ever had”. The Coalition has demonstrated its amity with a host of announcements, including the co-payment, which also affects diagnostic tests and prescription drugs. (These charges will be capped for children, low-income earners and the chronically ill.)
More people will pay the Medicare levy surcharge, and fewer will qualify for the private health insurance rebate. Billions of dollars have been cut from public hospitals, and the preventive health agency and other health promotion programs have been shut down. The savings will be directed to a medical research fund.
Dutton says that without these reforms, spiralling costs will jeopardise Medicare’s viability. ”The government is very keen to keep Medicare and strengthen it. To keep it universal, we have to make sure it’s affordable. In my view, Medicare is only sustainable if those people who have a capacity to pay contribute to the system.”
However, Professor John Deeble, one of the original scheme’s architects, says while costs have been rising, they’re manageable. Health spending by our governments is low compared with other wealthy countries. The Coalition’s planned changes, he says, are not really about the sustainability of Medicare. ”They just want to spend the money on something else, simple as that.”
The Medicare levy (currently 1.5 per cent of an average income) was introduced to help fund a universal healthcare scheme. If our health costs rise, the government can raise the levy, Deeble says. In that way, people’s contributions are determined by their capacity to pay – their income – not by how often they need treatment. By introducing co-payments instead, the government is embracing something fundamentally different: a ”user-pays” notion of fairness in health funding.
In Medicare’s first incarnation, when social security minister Bill Hayden introduced the bill to Parliament, he declared that its three motivating principles were ”social equity, universal coverage and cost efficiency”.
Although the full details of the Coalition’s reforms haven’t been released, public health experts have been unanimous: as a package, it’s simply bad policy.
”We’ve actually tried all these solutions before, which is why we know they don’t work,” says Boxall, who is the director of the Deeble Institute for Health Policy Research. ”We need to step back and look at the structural problems with our health system.”
Two key problems were unforeseen at the time of Medicare’s design: the rise of private healthcare, and the growing burden of chronic illnesses. ”Things have changed,” Boxall says. ”So what are we doing to improve universality, equity and efficiency?”
For most of the 20th century, Australia had a two-tier medical system: a very basic insurance system for the working class and a fee-paying model for those who could afford it. ”Doctors offered quite different services, and in many cases different waiting rooms for each group,” says Associate Professor James Gillespie, from the University of Sydney’s school of public health, co-author of Making Medicare.
The World Health Organisation says ”universal coverage” means ”all people have access to services and do not suffer financial hardship paying for them”.
But under Medicare, we’re already failing the equity test. More than one-in-six Australians say they don’t see a doctor or fill prescriptions because of the cost, according to an international study published by the journal Health Affairs. Other research has shown that people who live in poorer neighbourhoods are more likely to delay medical care.
Even without co-payments, Australian patients fork out a lot for treatment from their own pockets, compared with other developed countries. The two-tier system has re-emerged. One reason, says Gillespie, is that ”both sides of politics have refused to think seriously about the role of the private system”. Major reviews commissioned by both the Howard and Rudd governments specifically avoided examining its role.
When Medicare began, private hospitals were a small industry, run by churches and charities. But in the past two decades they’ve become a big business, where doctors earn much more.
Until the 1990s, private health insurance was in terminal decline. But spurred on by the Howard government’s incentives – the Medicare levy surcharge and lifetime cover discount – just under half the population now has private cover. ”We’ve ended up with a private system that shifts services away from the public and creates more privileged ways of doing things,” says Gillespie.
He says private funding can contribute to universal care, so long as core services are delivered the same way to everyone. Canada has a similar system to ours, but private insurance isn’t allowed to cover the services offered by its public system. ”If there’s a different system for those who can afford better, you end up with a residual service, which gets squeezed and becomes second best,” he says.
The Coalition argues the co-payment is a ”price signal” to alert people to the real cost of treatment. But there’s something unusual about healthcare – even economists say so. In simple terms: you can judge how you’ll feel if you forgo buying a hamburger, but not if you forgo visiting the doctor.
”In the case of healthcare, part of the product itself is giving you that information,” explains Professor Jeff Richardson, from Monash University’s centre for health economics. ”You’re not in a position to judge what life would be like with and without it.” All of which means that promoting efficiency is more complex than imposing a price signal.
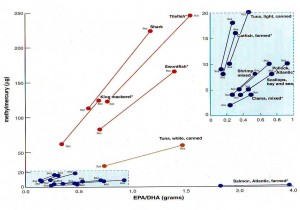
Australia’s health costs have been rising, but compared with other OECD countries our total health spending – both private and public – is just below average. It’s half that of the United States, as a percentage of GDP.
”When the government says Medicare is unsustainable, it’s lying,” Richardson says. ”The Australian government could spend much more on health if it wished. It’s simply a political and social judgment that it doesn’t want to.”
Curiously, despite Dutton’s warnings about unsustainable health spending, his reforms – which aim to push more people into the private system – will end up costing more overall. When the government acts as our single-insurer under Medicare, it has the power and incentive to bargain hard: as a result of bulk billing, GPs incomes are low by international standards. But with many different payers – like in the US system – it’s easier for private insurers to increase fees than control costs.
And for now, GPs and pharmaceuticals are the most cost-effective parts of the health system. Increasing their price will push more patients into hospitals, which are much more costly.
The measures are not a question of efficiency, Richardson says, but rather an ideological choice that health is an individual responsibility, not a shared one, like defence or policing. ”If we swing over to the private sector and push it back on individuals, the health of poorer people will suffer and overall costs will almost certainly rise.”
Dutton, however, maintains the measures aren’t about ideology, citing the Hawke government’s plans to introduce a $2.50 co-payment for GP visits in 1991. (Paul Keating scrapped the idea as prime minister.) ”I strongly believe that the changes we’ve put forward will improve access and the standard of care provided by GPs,” Dutton says.
But the biggest challenge to the standard of care now comes from an entirely different source, one his reforms do nothing to address. Our greatest healthcare inefficiency is found in a disconnect between the system – the fragmented network of hospitals, specialists and GPs, and their mishmash of state, federal and private funding – and the kinds of illnesses we have.
Where once we suffered acute ailments, we now need ongoing support with chronic conditions, says Dr Steve Hambleton, outgoing president of the Australian Medical Association. The number of deaths from heart attacks, for example, peaked in the 1970s. But living with heart disease requires continual treatment and adjustment, especially as you develop other conditions.
Patients with chronic diseases need to see a variety of health professionals and have frequent tests – but they are often seeing them in a piecemeal way with little continuity or communication between experts. Many of these, such as physiotherapists, psychologists or dieticians, are excluded or receive only limited funding under Medicare.
Both parties have attempted limited reforms to address the rise of chronic illnesses. But Hambleton says: ”We need a proactive, long-term approach … supporting primary healthcare to keep patients out of hospitals, and make sure people don’t fall through the cracks when they move between community and hospital care.”
The wide hallway of the Victorian Aboriginal Health Service in Fitzroy is humming: people young and old are waiting and chatting. Some are on the go, others hovering around a wood heater. Today, a specialist is visiting to conduct an ear, nose and throat clinic.
Jason King, the centre’s CEO, says they offer an holistic service. There are GPs, dentists, visiting specialists, social workers and financial counsellors, all supported by Aboriginal health workers. ”It’s not pumping them out every ten minutes. It’s ‘How’s mum and dad going? How’s uncle going who lives with you?’ We’re the central hub, this is where people come and see family.”
Last year, the health service celebrated its 40th anniversary. Each year, about a third of the state’s Aboriginal population pass through its doors. The centre’s model of integrated care, embedded in the values of its community, is exactly what doctors and experts have ordered – along with the WHO, the OECD and several Australian inquires.
But King says the co-payment and cuts to preventive health will either cost the centre patients or take a chunk out of its budget. Either way, that means fewer services.
There are 28 Aboriginal community-controlled health centres around the state. Jill Gallagher, CEO of their peak body, says Aboriginal health remains worse than the rest of the nation. ”The life expectancy in Fitzroy is the same as the life expectancy in Fitzroy Crossing,” she says. ”For every dollar spent on Medicare for a non-Aboriginal person, about 60¢ is spent on Aboriginal people. Access to primary healthcare is still not equitable, in spite of the fact there’s four times the burden of illness in the Aboriginal community.”
Dr Mary Belfrage, the service’s medical director, says any barriers to accessing healthcare cause people to show up later, with advanced conditions, which are more expensive to treat. ”It all translates to worse health outcomes, but it’s also inefficient,” she says. ”This isn’t about party politics or a particular budget. It’s about the principle of equity and how it impacts on health.”