All posts by blackfriar
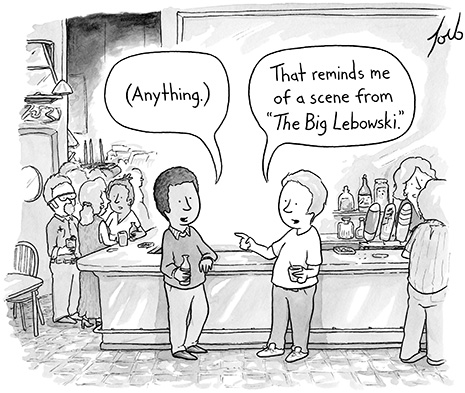
That reminds me of a scene from “The Big Lebowski”
I have no idea, I just write…
Punchy interview with Bill Gates’ favourite author. Alignment on food. Other things interesting, but unrelated.
http://www.wired.com/wiredscience/2013/11/vaclav-smil-wired/?mbid=synd_gfdn_bgtw
This Is the Man Bill Gates Thinks You Absolutely Should Be Reading
- BY CLIVE THOMPSON
- 11.25.13
- 6:30 AM
 Author Vaclav Smil tackles the big problems facing America and the world. Andreas Laszlo Konrath“There is no author whose books I look forward to more than Vaclav Smil,” Bill Gates wrote this summer. That’s quite an endorsement—and it gave a jolt of fame to Smil, a professor emeritus of environment and geography at the University of Manitoba. In a world of specialized intellectuals, Smil is an ambitious and astonishing polymath who swings for fences. His nearly three dozen books have analyzed the world’s biggest challenges—the future of energy, food production, and manufacturing—with nuance and detail. They’re among the most data-heavy books you’ll find, with a remarkable way of framing basic facts. (Sample nugget: Humans will consume 17 percent of what the biosphere produces this year.)His conclusions are often bleak. He argues, for instance, that the demise of US manufacturing dooms the country not just intellectually but creatively, because innovation is tied to the process of making things. (And, unfortunately, he has the figures to back that up.) WIRED got Smil’s take on the problems facing America and the world.
Author Vaclav Smil tackles the big problems facing America and the world. Andreas Laszlo Konrath“There is no author whose books I look forward to more than Vaclav Smil,” Bill Gates wrote this summer. That’s quite an endorsement—and it gave a jolt of fame to Smil, a professor emeritus of environment and geography at the University of Manitoba. In a world of specialized intellectuals, Smil is an ambitious and astonishing polymath who swings for fences. His nearly three dozen books have analyzed the world’s biggest challenges—the future of energy, food production, and manufacturing—with nuance and detail. They’re among the most data-heavy books you’ll find, with a remarkable way of framing basic facts. (Sample nugget: Humans will consume 17 percent of what the biosphere produces this year.)His conclusions are often bleak. He argues, for instance, that the demise of US manufacturing dooms the country not just intellectually but creatively, because innovation is tied to the process of making things. (And, unfortunately, he has the figures to back that up.) WIRED got Smil’s take on the problems facing America and the world.
You’ve written over 30 books and published three this year alone. How do you do it?
Hemingway knew the secret. I mean, he was a lush and a bad man in many ways, but he knew the secret. You get up and, first thing in the morning, you do your 500 words. Do it every day and you’ve got a book in eight or nine months.
What draws you to such big, all-encompassing subjects?
I saw how the university life goes, both in Europe and then in the US. I was at Penn State, and I was just aghast, because everyone was what I call drillers of deeper wells. These academics sit at the bottom of a deep well and they look up and see a sliver of the sky. They know everything about that little sliver of sky and nothing else. I scan all my horizons.
Let’s talk about manufacturing. You say a country that stops doing mass manufacturing falls apart. Why?
In every society, manufacturing builds the lower middle class. If you give up manufacturing, you end up with haves and have-nots and you get social polarization. The whole lower middle class sinks.
You also say that manufacturing is crucial to innovation.
Most innovation is not done by research institutes and national laboratories. It comes from manufacturing—from companies that want to extend their product reach, improve their costs, increase their returns. What’s very important is in-house research. Innovation usually arises from somebody taking a product already in production and making it better: better glass, better aluminum, a better chip. Innovation always starts with a product.
Look at LCD screens. Most of the advances are coming from big industrial conglomerates in Korea like Samsung or LG. The only good thing in the US is Gorilla Glass, because it’s Corning, and Corning spends $700 million a year on research.
American companies do still innovate, though. They just outsource the manufacturing. What’s wrong with that?
Look at the crown jewel of Boeing now, the 787 Dreamliner. The plane had so many problems—it was like three years late. And why? Because large parts of it were subcontracted around the world. The 787 is not a plane made in the USA; it’s a plane assembled in the USA. They subcontracted composite materials to Italians and batteries to the Japanese, and the batteries started to burn in-flight. The quality control is not there.
 Bill Gates’ actual bookshelf. We count six books by Smil in this section alone. Ian Allen
Bill Gates’ actual bookshelf. We count six books by Smil in this section alone. Ian Allen
Can IT jobs replace the lost manufacturing jobs?
No, of course not. These are totally fungible jobs. You could hire people in Russia or Malaysia—and that’s what companies are doing.
Restoring manufacturing would mean training Americans again to build things.
Only two countries have done this well: Germany and Switzerland. They’ve both maintained strong manufacturing sectors and they share a key thing: Kids go into apprentice programs at age 14 or 15. You spend a few years, depending on the skill, and you can make BMWs. And because you started young and learned from the older people, your products can’t be matched in quality. This is where it all starts.
You claim Apple could assemble the iPhone in the US and still make a huge profit.
It’s no secret! Apple has tremendous profit margins. They could easily do everything at home. The iPhone isn’t manufactured in China—it’s assembled in China from parts made in the US, Germany, Japan, Malaysia, South Korea, and so on. The cost there isn’t labor. But laborers must be sufficiently dedicated and skilled to sit on their ass for eight hours and solder little pieces together so they fit perfectly.
But Apple is supposed to be a giant innovator.
Apple! Boy, what a story. No taxes paid, everything made abroad—yet everyone worships them. This new iPhone, there’s nothing new in it. Just a golden color. What the hell, right? When people start playing with color, you know they’re played out.
Let’s talk about energy. You say alternative energy can’t scale. Is there no role for renewables?
I like renewables, but they move slowly. There’s an inherent inertia, a slowness in energy transitions. It would be easier if we were still consuming 66,615 kilowatt-hours per capita, as in 1950. But in 1950 few people had air-conditioning. We’re a society that demands electricity 24/7. This is very difficult with sun and wind.
Look at Germany, where they heavily subsidize renewable energy. When there’s no wind or sun, they boost up their old coal-fired power plants. The result: Germany has massively increased coal imports from the US, and German greenhouse gas emissions have been increasing, from 917 million metric tons in 2011 to 931 million in 2012, because they’re burning American coal. It’s totally zany!
What about nuclear?
The Chinese are building it, the Indians are building it, the Russians have some intention to build. But as you know, the US is not. The last big power plant was ordered in 1974. Germany is out, Italy has vowed never to build one, and even France is delaying new construction. Is it a nice thought that the future of nuclear energy is now in the hands of North Korea, Pakistan, India, and Iran? It’s a depressing thought, isn’t it?
The basic problem was that we rushed into nuclear power. We took Hyman Rickover’s reactor for submarines and pushed it so America would beat Russia. And that’s just the wrong reactor. It was done too fast with too little forethought.
You call this Moore’s curse—the idea that if we’re innovative enough, everything can have yearly efficiency gains.
It’s a categorical mistake. You just cannot increase the efficiency of power plants like that. You have your combustion machines—the best one in the lab now is about 40 percent efficient. In the field they’re about 15 or 20 percent efficient. Well, you can’t quintuple it, because that would be 100 percent efficient. Impossible, right? There are limits. It’s not a microchip.
The same thing is true in agriculture. You cannot increase the efficiency of photosynthesis. We improve the performance of farms by irrigating them and fertilizing them to provide all these nutrients. But we cannot keep on doubling the yield every two years. Moore’s law doesn’t apply to plants.
So what’s left? Making products more energy-efficient?
Innovation is making products more energy-efficient — but then we consume so many more products that there’s been no absolute dematerialization of anything. We still consume more steel, more aluminum, more glass, and so on. As long as we’re on this endless material cycle, this merry-go-round, well, technical innovation cannot keep pace.
Yikes. So all we’ve got left is reducing consumption. But who’s going to do that?
My wife and I did. We downscaled our house. It took me two years to find a subdivision where they’d let me build a custom house smaller than 2,000 square feet. And I’ll test you: What is the simplest way to make your house super-efficient?
Insulation!
Right. I have 50 percent more insulation in my walls. It adds very little to the cost. And you insulate your basement from the outside—I have about 20 inches of Styrofoam on the outside of that concrete wall. We were the first people building on our cul-de-sac, so I saw all the other houses after us—much bigger, 3,500 square feet. None of them were built properly. I pay in a year for electricity what they pay in January. You can have a super-efficient house; you can have a super-efficient car, a little Honda Civic, 40 miles per gallon.
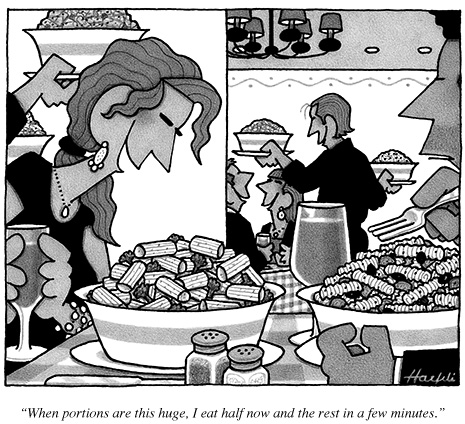
Your other big subject is food. You’re a pretty grim thinker, but this is your most optimistic area. You actually think we can feed a planet of 10 billion people—if we eat less meat and waste less food.
We pour all this energy into growing corn and soybeans, and then we put all that into rearing animals while feeding them antibiotics. And then we throw away 40 percent of the food we produce.
Meat eaters don’t like me because I call for moderation, and vegetarians don’t like me because I say there’s nothing wrong with eating meat. It’s part of our evolutionary heritage! Meat has helped to make us what we are. Meat helps to make our big brains. The problem is with eating 200 pounds of meat per capita per year. Eating hamburgers every day. And steak.
You know, you take some chicken breast, cut it up into little cubes, and make a Chinese stew—three people can eat one chicken breast. When you cut meat into little pieces, as they do in India, China, and Malaysia, all you need to eat is maybe like 40 pounds a year.
So finally, some good news from you!
Except for antibiotic resistance, which is terrible. Some countries that grow lots of pork, like Denmark and the Netherlands, are either eliminating antibiotics or reducing them. We have to do that. Otherwise we’ll create such antibiotic resistance, it will be just terrible.
So the answers are not technological but political: better economic policies, better education, better trade policies.
Right. Today, as you know, everything is “innovation.” We have problems, and people are looking for fairy-tale solutions—innovation like manna from heaven falling on the Israelites and saving them from the desert. It’s like, “Let’s not reform the education system, the tax system. Let’s not improve our dysfunctional government. Just wait for this innovation manna from a little group of people in Silicon Valley, preferably of Indian origin.”
You people at WIRED—you’re the guilty ones! You support these people, you write about them, you elevate them onto the cover! You really messed it up. I tell you, you pushed this on the American public, right? And people believe it now.
Bill Gates reads you a lot. Who are you writing for?
I have no idea. I just write.
nutrition and exercise, not dieting…
Plenty of sensible lines, though nothing about fasting…
http://bigthink.com/experts-corner/why-dieting-is-the-worst-way-to-lose-weight
Why Dieting is the Worst Way to Lose Weight
by TOM VENUTO NOVEMBER 23, 2013, 6:00 AM
Dieting is the worst way to lose weight. Most people would say I’m crazy for making such an outrageous claim. However, by the time you finish reading this short article, I think you’ll agree with me: Not only that, my hope is that you’ll agree so much that you’ll join me on my mission against “dieting” — at least the way the multi-billion dollar weight loss industry has been pushing it on everyone for years.
So what on Earth am I talking about, “dissing” dieting like that? Haven’t I said it myself many times before that diet is the most important factor for burning fat and keeping it off? Actually, no. That’s where the misunderstanding is. What I’ve said is that if I were to put the many elements of successful fat loss into the order of their priority, nutrition would be at the top of the list.
There’s a big difference between “diet” and “nutrition”
You may see where I’m going with this now, but you also might be wondering if this is just semantics. Yes, it is. But that’s precisely why “diet” and “nutrition” are not saying the same thing. Words are loaded with meaning between the lines. Being successful is about understanding the power of words — and using the words that successful people use.
Few words are more semantically loaded than diet. Think about what connotations — and whether they are positive or negative. What comes up when you think of diet?
Restriction
Forbidden foods
Banned food groups
What you can “never eat”
Hunger
Gimmicks
Fads/trends (that pass or come and go in cycles)
Quick fixes (often unhealthy or dangerous)
The word “diet” was supposed to simply describe the way a person eats. “Diet” comes from the Latin, diaeta, meaning “way of life.” But in our technologically advanced, sedentary society today, and with the obesity crisis we’re facing, and the multi-billion dollar industry it has spawned, the word “diet” has become tainted . . .
Today, I think ‘diet’ carries too much negative baggage to use so loosely. The way I define it, a diet is any unsustainable change in your eating behavior to try to lose weight. When you say you’re going on a diet, you’re also saying that at some point you’re going off it. While you’re on it, you suffer all those negative associations I mentioned above.
By contrast, think about the connotations of the word nutrition. Do you think of anything negative? I don’t. I think of:
Vitamins
Minerals
Micronutrients
Fiber
Muscle-building protein (amino acids)
Unrefined foods, closer to their form in nature
Energy
Vitality
Health
Now think of the word program. A program implies that there is structure. So I define a nutrition program as a structured plan you can follow as a lifestyle, which nourishes you with nutritious food that helps you get leaner, stronger, fitter and healthier . . . and stay that way.
I propose we replace “diet” with “nutrition program” unless we are specifically talking about something short term.
I believe this distinction in words is crucial, but just to play devil’s advocate, let’s assume that diet and nutrition program mean exactly the same thing. There’s still a huge problem with the diet alone approach, and therefore, why 99% of the entire weight loss industry is wrong:
Diet is only one of the elements needed for a leaner, stronger, fitter, and healthier body. There are three other elements that most people are missing.
Dieting might improve your health. On the other hand, depending on your approach to “diet,” it might destroy your health. Dieting is not always healthy. Nutrition and training together is a sure-fire pathway to health.
Weight loss diets fail 80-95% of the time. Not because they don’t take the weight off, but because they rarely keep it off. Most dieters relapse. Drug addicts and alcoholics in rehab have a higher success rate than that.
Exercise and an active lifestyle are vital for long term weight loss maintenance.
The right kind of exercise is also vital for re-shaping your body . . .
Weight Loss Versus Body Transformation
There’s a world of difference between losing weight and transforming your body.
Dieting can’t transform your body. Only training can do that.
Dieting can’t make you stronger. Only training can do that.
Dieting can’t make you fitter. Only training can do that.
With diets, you might fit into smaller clothes. But you also may become a smaller version of your old self… a skinny fat person . . . weighing less . . . but still flabby (and weak).
The Muscle Loss Epidemic
With diet alone, 30 to 50% of your weight loss could come from lean body mass. And if you’re getting older, the prospect of losing muscle and strength should genuinely frighten you.
After age 50, you lose 1-2% of your lean muscle every year if you do nothing (if you’re not resistance training). After age 60, you lose up to 3% per year.
Let’s suppose you’re 50 or 60 and you’re thinking, “A few percent of my lean mass? What’s the big deal? I have no desire to look muscly.” I can understand that. Your goals and values do change as you get older. But I already realize that most people don’t want to look like bodybuilders. However, gaining lean muscle, strength and fitness will improve the quality of anyone’s life.
Maintaining the muscle you have must be a priority for everyone because losing lean mass every year means losing your mobility and losing your independence as you get older.
Stop the Diet Insanity!
Given these facts, it’s sheer insanity that we have millions of people who want to lose weight — for health and for happiness — and the first thing or only thing they think of as a solution is DIET. They’re asking for deprivation, hunger, missing out on favorite foods, loss of muscle, loss of strength and eventually, loss of independence, putting a burden on other people to take care of them.
I’m not being melodramatic. I’m on mission to expose the mistakes of the dieting mentality and promote the benefits of the muscle-building, fitness and nutrition lifestyle.
The good news is, there’s a right way to burn fat and transform your body, but it’s not a one-trick show. You have to put several pieces together. This is total lifestyle change, so it’s not easy. But it is worth it.
This is as near to a miracle formula as you will ever find. It’s the 4 elements of the Burn the Fat, Feed the Muscle approach:
Nutrition program
Resistance (strength) training
Cardio Training
Mental training
Dieting is the worst way to lose weight
Not only that, here’s the nail in the coffin for 99% of what the weight loss industry is telling you: weight loss is the wrong goal to begin with. Burning the fat and keeping the muscle is the right goal. Even better, the right goal is to get leaner, stronger, fitter and healthier.
Train hard, and expect success.
© 2013 Tom Venuto, author of Burn the Fat, Feed the Muscle: Transform Your Body Forever Using the Secrets of the Leanest People in the World
Author Bio
Tom Venuto is a fat-loss expert, transformation coach and bestselling author of Burn the Fat, Feed the Muscle. Tom holds a degree in exercise science and has worked in the fitness industry since 1989, including fourteen years as a personal trainer. He promotes natural, healthy strategies for burning fat and building muscle, and as a lifetime steroid-free bodybuilder, he’s been there and done it himself. Tom blends the latest science with a realistic, commonsense approach to transforming your body and maintaining your perfect weight for life.
For more information please visit http://www.burnthefatblog.com/ and http://www.burnthefatfeedthemuscle.com/ and follow the author on Facebook and Twitter
SMS provides for an effective weight loss intervention
Citation: http://www.jmir.org/2013/11/e244/
Study: Texting effective intervention tool for weight control
 Daily text messaging may be a useful self-monitoring tool for weight control, particularly among racial/ethnic minority populations most in need of intervention, according to Duke University study results published in a Journal of Medical Internet Research article.
Daily text messaging may be a useful self-monitoring tool for weight control, particularly among racial/ethnic minority populations most in need of intervention, according to Duke University study results published in a Journal of Medical Internet Research article.
“Recent studies show that racial/ethnic minorities are more likely than white individuals to own mobile phones,” states the article. “The high familiarity with and penetration of mobile technologies makes text messaging an ideal intervention platform among these populations.”
The purpose of the randomized controlled pilot study was to evaluate the feasibility of a text messaging intervention for weight loss among predominantly black women, who “have alarmingly high rates of obesity as compared with other gender and racial/ethnic groups.” The secondary aim of the study was to evaluate the effects of the intervention on weight change relative to an education control arm.
Fifty obese women aged 25-50 years were randomized to either a six-month intervention using a fully automated system that included daily text messages for self-monitoring tailored behavioral goals (e.g., 10,000 steps per day, no sugary drinks) along with brief feedback and tips (26 women) or to an education control arm (24 women). The article states that weight was objectively measured at baseline and at six months, while adherence was defined as the proportion of text messages received in response to self-monitoring prompts.
At six months, the article reports that the intervention arm lost a mean of 1.27 kg, and the control arm gained a mean of 1.14 kg. The average daily text messaging adherence rate was 49 percent with 85 percent texting self-monitored behavioral goals two or more days per week. Moreover, about 70 percent strongly agreed that daily texting was easy and helpful and 76 percent felt the frequency of texting was appropriate.
“Given that the majority of evidence indicates that greater adherence leads to better outcomes, our study suggests that mHealth-based approaches to self-monitoring may enhance engagement and reduce the burdens commonly associated with other modes,” concluded the article. “Our intervention was relatively low intensity and has greater potential for dissemination compared to higher intensity interventions. As technology penetration increases in the target population, the use of this modality will become increasingly relevant and helpful as an intervention tool for weight control.”
Earlier this year, an article published in the Journal of American Medical Informatics Association revealed that mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in a weight loss program are more effective than traditional methods. The study involved a post hoc analysis of a six-month randomized weight loss trial among 96 overweight men and women, which found that physical activity app users self-monitored exercise more frequently over the six-month study and reported greater intentional physical activity than non-app users.
To learn more:
– read the article in JMIR
Building a bridge to the future with population health analytics…
- Leading US providers are using analytics to bring a more intense focus on gaps in care, to discover cost outliers, and to put a magnifying glass on efficiency
- “Unlike other industries that may be high users of data and very sophisticated, the healthcare industry is at a different point”
- “A platform where we mesh both claims data and data out of our electronic health records allows a lot more to be learned. The type of intelligence that we can glean is at a much more informed level than if we’re just dealing with one of those data sets in isolation.”
- At the heart of population health analytics is the concept of risk stratification: understanding, through various inputs such as claims data, surveys, and EHRs, which members of a given healthcare organization’s customer base represent a level of risk for which intervention offers the greatest possibility of preventing future hospital admissions, reducing readmissions, improving overall health, and lowering costs.
- Cleveland Clinic’s Explorys pulls data from a variety of sources—multiple electronic health records, billing systems, claims data from CMS and other payers—and assimilates that all together to allow filtering, reporting, identify care gaps and registry functions
- A variety of tools exist to help stratify risk:
> Some tools place members of a population on a scatter plot to make the identification of outliers easier
> Other tools organize a population into patient registries to track various diseases and treatments
> Still other tools use input gathered from patient surveys.
- near-real time data is an important addition
How Population Health Analytics Opens Opportunities for Better Care
Scott Mace, for HealthLeaders Media , November 20, 2013
Innovators are blending technology with new care models while targeting high-risk patients in a patient-centered strategy.
This article appears in the November issue of HealthLeaders magazine.
Without robust analytics technology, the goals of accountable care and population health cannot fully be achieved, good intentions notwithstanding. ACOs must correlate clinical data and claims data and use analytics technology to produce the actions needed to manage the health of a population. The data is there, but the healthcare industry does not have an evenly distributed knowledge of how to use it effectively.
With potential savings of up to $300 billion a year, according to the consulting firm McKinsey & Company, the upside of industrywide analytics to manage a population is considerable.
And, increasingly, providers have the raw data they need to feed an analytics system. But it is not as simple or quick as installing electronic health record technology—no small feat in itself for many organizations—and must be accompanied by solid governance and education, according to leading providers.
These providers are using analytics to bring a more intense focus on gaps in care, to discover cost outliers, and to put a magnifying glass on efficiency. But the use of such healthcare analytics has yet to reach maturity.
Early in the process
“Our organization is facing what most of the industry is facing, and that is the need to build a bridge to the future through analytics; so unlike some other industries that may be high users of data and very sophisticated, the healthcare industry is just in a different point,” says Aric Sharp, vice president of the accountable care organization at UnityPoint Health, a West Des Moines, Iowa–based integrated health system with 3,026 licensed beds across 15 hospitals and total operating revenue of $2.7 billion.
“We’re still in the process, as an industry, of going through implementing electronic health records and achieving meaningful use and those types of things. At the same time, with a lot of the new efforts around accountable care organizations, for one of the first times many providers have an opportunity to collect claims data by working with payers,” Sharp says. “We felt it necessary to build a platform where we can mesh together both claims data and data out of our electronic health records, because there’s a lot more that’s able to be learned in that type of an environment. The type of intelligence that we can glean is at a much more informed level than if we’re just dealing with one of those data sets in isolation.”
UnityPoint Health typifies numerous providers, having initiated analytics for its population health initiative only a couple of years ago. “The primary lesson is, this is really difficult, and there’s a lot to learn along the way,” Sharp says. “And yet, we can certainly see that as we continue to enhance the work, there’s more and more benefit with every step. The big learning is that there’s just a lot to be learned, and it’s exciting, because with every step of the process, we are better able to identify opportunities to improve care, and we’re able to become more efficient at this type of work.”
At the heart of population health analytics is the concept of risk stratification: understanding, through various inputs such as claims data, surveys, and EHRs, which members of a given healthcare organization’s customer base represent a level of risk for which intervention offers the greatest possibility of preventing future hospital admissions, reducing readmissions, improving overall health, and lowering costs.
UnityPoint Health selected analytics technology from Explorys, a data spinoff of Cleveland Clinic founded in 2009.
“Explorys is able to pull data from a variety of sources—multiple electronic health records, our own billing systems, claims data from CMS or other payers—and assimilate that all together,” Sharp says. “Explorys is really what sits on top of that and gives us an ability to slice and dice and analyze it and probe it and report quality metrics, identify gaps in care, and in the future even use that to do outreach to patients and do registry-type functions.”
UnityPoint Health still counts the time until the big payoff in years. “We’re not yet ready to say that it has an impact on our global per-member per-month spent,” says Vice President of Operations Kathleen Cunningham. “It will, but we are so early in our innovation that some of our results are really based on the pilot type of innovation programs that we’re working on.”
Starting with employee populations
In many healthcare systems, population health analytics success stories are just beginning to emerge, but some providers have used their own employee populations as a proof of concept for the effectiveness of the effort.
For the past 11 years, employees of Adventist HealthCare—a nonprofit network based in Gaithersburg, Md., with three acute care and three specialty hospitals, 6,263 employees, and 2012 revenue of $726 million—have been managed for risk by the self-insured provider.
“It got started with the idea that a healthier population is going to be a more effective employee population, and it’s going to also be a lower-cost population,” says Bill Robertson, president and CEO of Adventist HealthCare.
A decade ago, Adventist started working with InforMed Healthcare Solutions, since acquired by Conifer Health Solutions, to use InforMed’s set of data warehouse tools to improve its health plan design and determine where interventions were needed, Robertson says. Adventist and InforMed worked collaboratively to develop those tools and restructure the Adventist workflow to ramp up the effectiveness of the population health program.
As a result of population analytics, as well as other measures such as discouraging tobacco use and encouraging use of generic drugs, the inflation rate of Adventist’s employee health plan cost over the past nine years was half the national average, Robertson says.
A key development in the population health initiative came in 2005, when Adventist created personal health nurses as part of a pilot patient-centered medical home to work with the approximately 360 high-risk members of Adventist’s 6,600 employee-based covered lives identified by the InforMed data tools, Robertson says.
In a pilot, Adventist selected 27 of 50 high-risk patients (54%) and was able to move them out of the high-risk pool into moderate or low-risk pools, and it achieved a 35% reduction in the cost of care for that population, he says.
According to Adventist, the pilot project that achieved the 35% reduction did reduce health plan costs by $381,000 among the 27 patients who moved from the high-risk pool. The amount expended to achieve this 35% reduction was only $31,000, so every dollar spent returned approximately $12 in savings.
“It was actually so dramatic that it brought the inflation rate on our health plan to zero in that year,” Robertson says. “We were pretty pleased with that.” Overall, Adventist has saved “tens of millions of dollars” due to employee population health analytics to reshape the program and services for employees, he says.
Adventist then expanded this pilot PCMH to 5% of its employees (roughly 360 people), and continues to see the same kind of positive outcomes, Robertson says. Nurses make up the majority of InforMed users.
Three years ago, Adventist created ACES, which stands for Ambulatory Care EHR Support, an initiative to move its ambulatory physicians to use electronic medical records to expand its capacity to do population-focused care. By the end of 2013, more than 400 physicians will be using the ACES system. “So much of the job is how you integrate care across physicians and across the delivery system,” Robertson says. “When you have one person who’s seeing 15 physicians, but each physician thinks they’re the only one, you end up with different challenges than when you can see everything.”
All physicians who are participating providers in the Adventist HealthCare employee health benefit plan have access to the InforMed tools and analytics. Only a limited number directly access the information because the personal health nurses provide most of the ongoing care management, with the physicians serving more as the team captains, Robertson says.
The next step for Adventist IT is to tie analytics with the employee EHR. “What we’re morphing toward is linking all of this together with HIE infrastructure so that the information that is in the InforMed platform will be available in your EHR platform and vice versa through the information exchange,” Robertson says.
Adventist also created financial incentives that help its physicians spend “all the time it takes” to manage high-risk patients, Robertson says. “With an ACO, you don’t really get paid an incentive until you’ve been successful—at least after the first year you’ve demonstrated that things are working and that they’re [generating] shared savings,” he says. “So we’re still in the process of sorting out how we’ll make sure this infrastructure is utilized actively.”
Detailing the financial incentives, Robertson says the primary care physicians who participate in the patient-centered medical homes receive additional compensation, such as a monthly retainer or hourly incentive to compensate them for the additional time that is necessary to care for the high-risk patients in the PCMH.
Recent headlines have highlighted some fallout from the Pioneer ACO program. Fifteen charter members dropped out of the program after finding inadequate return on investment or improvement from their ACO initiative. To Robertson, this just highlights the importance of population health analytics in achieving ACO success. Had Adventist focused on no-risk or low-risk populations, it might not have achieved nearly the cost savings it had with its own proof of concept by targeting the high-risk pool of its self-insured employee-based covered lives, he says.
Now Adventist is forming an ACO for Medicare populations based on this same set of tools to track high-risk members of those populations. As time goes on, commercial-payer populations are also in Adventist’s sights. “We have a couple of pilots, like an apartment building that has a very large population of higher-risk individuals that we’re providing those types of services to, and it’s interesting to see when you focus on it what you achieve in terms of reduced consumption of healthcare services and increased health status,” Robertson says.
Leading the way to better patient care
At Virtua Health, population health analytics from Alere Analytics is being implemented to determine the highest-risk patients from a cohort of 12,000 attributed Medicare lives, says James Gamble, MD, chief medical information officer of the four-hospital, 885-staffed-bed integrated delivery network headquartered in Marlton, N.J.
Virtua became an ACO on January 1 and is preparing to add another 14,000 covered lives with a commercial insurer, says Alfred Campanella, Virtua’s executive vice president of strategic business growth and analytics.
“There are lots of different scenarios where action is needed to prevent an admission or to prevent a condition from getting worse,” Campanella says. Virtua is working with Alere to publish its alert lists via a Microsoft Dynamics customer relationship management platform. “That allows care nurses to take advantage of our Microsoft products like email and word processing,” he adds.
Virtua uses RNs to provide close case management of the high-risk population. Meanwhile, 80 Virtua-employed primary care doctors are kept updated via the workflow into the system’s electronic health record software. “That way that doctor doesn’t have to leave their EMR or jump around to see where things are going,” Campanella says.
“Our initial focus,” Gamble explains, “will be on these high-risk patients, so as we see it, these case managers’ day-to-day job will be: They’ll have a patient load, they will have care plans, they will have activities assigned to them for these patients.”
But the physician does not need to be the primary manager.
“As long as patients are following care plans, which are developed and approved by the providers, then the nurses will be managing them,” Gamble says. “Their communication will be more as updates. When an alert arises that the patient is at risk or in trouble, then obviously the nurse would directly communicate with the physician to try to intervene at any early stage before the patient’s health deteriorates or the patient ends up in the emergency room of the hospital.”
“What we’re seeing now is a more intense focus to try to fix those gaps in care and to identify patients who are at high risk for hospitalization or readmission or who need special attention,” Campanella says. “Technology gives you a greater magnifying glass in many respects for seeing the barriers to care and for creating efficiencies in care delivery. While all the analysis is not complete, early results for clinical and financial savings are promising.”
Support from top leadership has been crucial to Virtua’s transformational pivot toward analytics. “This whole idea of care coordination was approved at the board of trustees level,” Campanella says. “We’ve had tremendous support from our CEO, Richard Miller. One of our senior vice presidents, Stephen Kolesk, MD, doubles as the president of this subsidiary that is the ACO. He has a title of senior vice president for clinical integration, so it’s very tightly integrated with the physicians.”
Technical design of the Virtua analytics solution is close to completion. Parts of it will deploy before the end of 2013, and other parts will roll out in the first quarter of 2014, says Campanella. Also part of the project are an existing health information exchange and a new patient portal built on top of the HIE, he adds.
“Innovation does require some experimentation and risk,” Campanella says. “The ones who are leaders are taking on some risk and putting some investment in without fully understanding the full picture, but that’s what makes them leaders.
“It’s now the right way to care for patients, to have this high touch, high visibility into all the different domains of their care and the handoffs between those domains, and so even if the ACO concept from a regulatory standpoint goes away, it’s still the right way to care for patients,”
Campanella says.
Outside the hospital walls
Organizations beyond postacute hospitals are also engaging healthcare in a variety of ways that have broad implications for how analytics will be deployed in healthcare across the United States.
Brentwood, Tenn.–based Brookdale Senior Living owns and operates about 650 senior living communities in 36 states. In 2012, Brookdale, through a partnership with the University of North Texas Health Science Center and Florida Atlantic University, received $2.8 million of a $7.3 million Centers for Medicare & Medicaid Services Health Innovations Challenge grant for population health management. The program expects to save more than $9 million over a three-year period.
Initially, Brookdale is focusing on population health at 27 communities in Texas and Florida, but by the end of the three-year grant, it will involve 67 communities, says Kevin O’Neil, MD, chief medical officer of the organization.
The CMS grant sets a goal for Brookdale of reducing avoidable hospital readmissions by 11%, O’Neil says. “We know we’re going to be focusing on certain quality metrics in addition to readmissions,” he says. “We’ll focus on dehydration rates, as well as new incidents of pressure ulcers, some of the major problem areas in geriatric care, and then, based on the data that we receive from the analytics tool, it’ll help guide our quality improvement teams in terms of the type of improvement efforts that need to be initiated.”
A variety of tools exist to help stratify risk. Some tools place members of a population on a scatter plot to make the identification of outliers easier. Other tools organize a population into patient registries to track various diseases and treatments. Still other tools use input gathered from patient surveys. A recent study, however, reported that many of those tools had not performed very well.
At St. David’s Health System in Austin, which is working with Brookdale on the challenge grant, 60% of readmissions recently were measured as coming from low-risk groups. “To me [this] means either that people hadn’t been stratified properly, or that they were being sent home when they probably did need some kind of service or follow-up,” O’Neil says.
The biggest hurdle in O’Neil’s experience with population health analytics has been engaging with the hospital C-suite to craft the business associate agreements necessary to manage populations. “Once we’ve developed a relationship with one entity and had success, it’s much easier to engage other entities within that system.”
In dealing with the two universities, O’Neil says, “We had to resolve some issues related to intellectual property to incorporate INTERACT into electronic information systems,” he says. INTERACT is an acronym for Interventions to Reduce Acute Care Transfers, a free quality improvement program for which FAU holds the trademark and copyright. “This has been resolved through a licensing agreement—Loopback [a Dallas-based analytics platform vendor] also has a licensing agreement with FAU to bake INTERACT tools into software programs.”
Both Brookdale and its hospital partners are using a common population health analysis dashboard and software provided by Loopback Analytics. “As a geriatrician, this is the most exciting time in my career, because I’ve always felt that fee-for-service medicine was the bane of good geriatric care because it rewarded volume rather than quality,” O’Neil says. “Having that near-real-time data is really going to be extremely helpful to us.”
Analytics and meaningful use
Analytics tools produce the patient registries that identify gaps in care, not just to meet ACO objectives, but also to meet the requirements of meaningful use stage 2, which takes effect in 2014, says Gregory Spencer, MD, a practicing general internist and chief medical officer at Crystal Run Healthcare, a multispecialty practice with more than 300 physicians based in Middletown, N.Y.
“There are frequently registry functions within EHRs, but the EHR is set up at the patient level,” Spencer says. “It’s not optimized for reporting groups of patients, so to kind of get that rollup, you have to have another layer on top of that to gather it up.”
Thus, some sort of aggregator function is needed. “Usually that is not something that many EMRs do well,” Spencer says. “Registries are mostly condition- or disease-specific lists of patients who satisfy a certain criteria: diabetics, patients with vascular disease, kids with asthma. Care gaps look at all patients who have not had a certain recommended service. There is overlap with the registries, since a list of patients due for their colonoscopy is a kind of registry that needs to be ‘worked’ to get those patients compliant.”
Like numerous other healthcare organizations, Crystal Run’s first foray into population health analytics employed Microsoft Excel spreadsheets.
“The basics can be done with available tools,” Spencer says. “People shouldn’t wait for the killer app that’s out there that’s fancy and has a slick user interface. You can really do a lot with what you have, probably immediately.”
Since 1999, however, Crystal Run has incrementally left Excel behind and built population health analytics reporting tools on top of its NextGen electronic health record software, Spencer says. Crystal Run also adopted the Crimson Population Risk Management service from the Advisory Board Company, which incorporates technology from Milliman Inc. on the back end, he says.
Like other providers, Crystal Run saw the shift coming from fee-for-service to accountable care and took early opportunities to get its hands on claims data and learn how to work with it, Spencer says.
Other resources offering insight to accountable care analytics were the Group Practice Improvement Network and the American Medical Group Association, where Spencer has been able to network with peers who have been pursuing population health analytics longer than Crystal Run has.
The Crystal Run practice, formed in 1996, grew out of a single-specialty oncology practice and today has 1,700 employees. It is designated by the NCQA as a level 3 patient-centered medical home, and in 2012, Crystal Run became one of the first 27 Medicare Shared Savings ACOs.
Analytics have revealed “a lot of surprises at who you think has been getting most of their care from you,” he says. Snowbirds—typically someone from the Northeast, Midwest, or Pacific Northwest who spends substantial time in warmer states during the winter—are receiving significant amounts of care that had been outside of Crystal Run’s knowledge.
But with Medicare claims data examined through its analytics services, Crystal Run has had its eyes opened to previously unobserved cost centers. For instance, the No. 1 biller of pathology services for a 10,000-patient Crystal Run cohort was discovered to be a local dermatologist.
“What it’s all about is improving quality and eliminating waste,” Spencer says. “That waste is [in] tests that aren’t really required [and even some] visits that are [being required]. It’s your habit and custom to see people back at a certain frequency, but when you really start thinking about it, do you really need to see somebody back every three months who has stable blood pressure and has been rock solid? Well, probably not. And so you start doing things like that, and it adds up incrementally.”
Crystal Run is able to incorporate patients’ outside visits to providers, Spencer says, “but it’s not easy. We require source documentation to satisfy measures. For example, we scan outside mammogram results into a directory that we can then report against. We don’t take people’s word for dates. We need to have the document.”
Getting the initial claims data from CMS took three months, and then it takes another three or six months’ worth of that data for it to become actionable, Spencer says.
Claims data on any one patient is also plagued by incurred but not reported claims. Until IBNR claims get processed through Medicare or other payers, a true picture of a patient’s treatment is incomplete.
In light of this, it’s important for all concerned to have realistic expectations of what population health analytics can achieve and when, Spencer says.
“Cost is a practical concern we all face in our day-to-day lives,” he says. “You get more for more money, but as in all things, you have to be prudent. I don’t know how you will be able to do business in the very near future without using some form of analytics. How will your quality measures be good enough to meet the ‘gates’ required for contracts? How will you know where you are or if you can grow and how? It has cost a lot of money—money that’s been spent over a long period of time. The cost is into the low millions.
“That said,” Spencer adds, “we are able to take advantage of newer payment models that reward us not just for healthcare, but outcomes. We can potentially get paid for not doing anything—the PMPM that can be negotiated when you show you are doing a good job managing a population of patients.”
Analytics in the ambulatory practice
Gastroenterologist Tom M. Deas Jr., MD, practices as part of North Texas Specialty Physicians based in Fort Worth, an independent physician association comprising nearly 600 family and specialty doctors. NTSP has its own health plan and has been managing Medicare patients at risk for several years.
NTSP provided initial funding for a population health analytics firm, Sandlot Solutions, which has now been spun out as a separate company, although NTSP remains a part owner and Deas also serves as Sandlot’s chief medical officer. NTSP uses Sandlot’s analytics software to manage 80,000 at-risk lives, Deas says.
“Without some of the information technology to identify those patients based on their illnesses, comorbid illnesses, their severity of illness, who their physicians are, where they’ve been going to get their care, and being able to manage the whole spectrum of the care, you’re at a serious disadvantage,” Deas says.
Sandlot’s technology combines claims and clinical data into a robust patient data warehouse that helps meet some of the quality measures required to be an ACO, says Deas. “With the ACO, no matter how much money you save, you don’t get a dime of it if you haven’t met all the quality measures, so if we fall short in that area, it’s economically not good and it’s not good for the patients.”
By default, all Pioneer ACOs received three years of Medicare claims data. Getting the data into the warehouse requires overcoming some well-known healthcare IT issues, such as reconciling that claims data with an enterprise master-patient index, eliminating duplicates, and general patient-matching issues, Deas notes.
Once that was done, NTSP could concentrate on using Sandlot’s analytics to spot and eliminate wasteful services, as such home visits for patients lacking a medical necessity for such visits, Deas says. Analytics-driven interventions can manage a few hundred overutilizers of services as outpatients, focusing care management on them, he adds.
After a year’s effort, NTSP has bent its cost curve through these efforts to the tune of $50 per member per month, Deas says. “Now we’re not completely there,” he cautions. “It’s an incremental process, because you’re not only doing management, but you’re changing behaviors also. You’re trying to get patients aligned with the primary care physician, trying to move them from one source of care that was maybe excessive utilization to another.”
Deas says measuring the ROI of analytics technology remains elusive.
“A lot of people think they just buy an analytics tool and a data warehouse and an HIE and it’ll sit there and solve their problems,” he says. “That is not the case. You have to have human folks using that tool to manage the care of patients, to lower the cost and improve the quality. It’s like me asking you how much more efficient are you with a smartphone than you were five years ago with whatever version of phone you had then. You can’t answer that question. All you know, it’s just one part of what’s happened in the past five years to make you more efficient.”
It no doubt helps that NTSP’s executive director, Karen van Wagner, has a PhD in statistics, giving the organization added expertise to quantify results as they emerge.
Analytics technology is just beginning to make its impact felt in population health management. Careful consideration of products, objectives, workflows, and business conditions will steer providers through potential pitfalls, but the effort is considerable and the challenge to healthcare leadership is ongoing.
“Among the things that made these changes successful is an IT infrastructure that supports population health management and care management,” Deas says. “We still have to throw a fair amount of resources—human resources—at it to make it work.”
Reprint HLR1113-2
This article appears in the November issue of HealthLeaders magazine.
Scott Mace is senior technology editor at HealthLeaders Media.
A behavioural economist’s view on obesity…
This is a typically obtuse, academic view of obesity, breathlessly attempting to cite the immense complexity of the disease, capping it with a plea for more research dollars, or at least a reallocation of research dollars.
There are a couple of interesting snippets:
- pets are also getting obese – 58.3% of cats were obese in 2012
- lab animals too are getting obese – 11.8% per decade from 1982 to 2003
- is this due to antibiotic-mediated changes to gut bacteria that not just change how we digest, but also how we behave?
- socially mediated effects?
So surprising that a behavioral economist’s view could be so dismal.
Source: http://www.nytimes.com/2013/11/10/business/the-co-villains-behind-obesitys-rise.html?_r=2&
The Co-Villains Behind Obesity’s Rise

Researchers have compared tissue samples from obese mice with those of normal mice to try to determine which behavioral or biological factors might cause humans to gain weight. Here, a 2012 experiment in Leipzig, Germany.
By SENDHIL MULLAINATHAN
Published: November 9, 2013
Why is obesity soaring? The answer seems pretty clear. In 1955, a standard soda at McDonald’s was only seven ounces. Today, a medium is three times as large, and even a child’s-size version is 12 ounces. It’s a widely held view that obesity is a consequence of our behaviors, and that behavioral economics thus plays a central role in understanding it — with markets, preferences and choices taking center stage. As a behavioral economist, I subscribed to that view — until recently, when I began to question my thinking.
For many health problems, of course, behavior plays some role but biology is often a major villain. “Biology” here is my catchall term for the myriad bodily mechanics that are only weakly connected to our choices. A few studies have led me to wonder whether the same is true with obesity. Have I been the proverbial owner of a (behavioral) hammer, looking for (behavioral) nails everywhere? Have I failed to appreciate the role of biology?
A first warning sign comes from looking at other animals. Our pets have been getting fatter along with us. In 2012, some 58.3 percent of cats were, literally, fat cats. That is taken from a survey by the Association for Pet Obesity Prevention. (The very existence of this organization is telling.) Pet obesity, however, can easily be tied to human behavior: a culture that eats more probably feeds its animals more, too.
And yet, a study by a group of biostatisticians in the Proceedings of the Royal Society challenges this interpretation. They collected data from animals raised in captivity: macaques, marmosets, chimpanzees, vervets, lab rats and mice. The data came from labs and centers and spanned several decades. These captive animals are also becoming fatter: weight gain for female lab mice, for example, came out to 11.8 percent a decade from 1982 to 2003.
But this weight gain is harder to explain. Captive animals are fed carefully controlled diets, which the researchers argue have not changed for decades. Animal obesity cannot be explained through eating behavior alone. We must look to some other — biological — driver.
Fittingly, the study is titled “Canaries in the Coal Mine.” Could our inability to explain animal obesity with behavior be a warning sign? Perhaps we are also overlooking biological drivers for human obesity. But what might these culprits be?
A particularly interesting candidate resides in your gut. Your digestive system is actually a complex ecosystem, playing host to hundreds of species of bacteria that do things as diverse as fermenting undigestedcarbohydrates and providing vitamins. They also regulate how much fat your body stores.
Not everyone, however, has the same gut bacteria. And, interestingly, the composition of this bacteria correlates with obesity. Of course, this relationship could be simple: the obese eat differently, and therefore they have different bacteria.
But a recent study in the journal Science showed that cause and effect could go the other way as well. Researchers harvested bacteria from pairs of human twins, where one twin was obese and the other was not. Then they transplanted these bacteria into mice. The mice who received bacteria from the obese twin gained weight, while the others did not. The mice did not eat more: Their metabolism changed so that they put on more weight even with the same caloric input.
What, then, determines your gut bacteria? It could be antibiotics or environmental toxins or how processed your food is. Another possibility is raised by a study in The New England Journal of Medicine that shows that obesity seems to “spread” across social networks, with people infecting their friends and neighbors. I had always assumed that was because birds of a feather flock together — and that is surely part of the explanation. But because gut bacteria can also spread among people in close proximity, perhaps the obesity epidemic really is, well, an epidemic?
I’m not arguing that behavior does not matter. Biology and behavior often interact; the spread of flu depends on whether we wash our hands. Similarly, the bacteria study found that the “obese gut bacteria” had an impact only when the mice were fed diets heavy in saturated fats.
Perhaps most interestingly, changing biology may even be changing cravings. Some biologists have hypothesized that our gut bacteria actually drive cravings for certain unhealthy foods. A focus on biology doesn’t mean a reduced emphasis on behavior, just a richer understanding of it.
These and other studies raise important possibilities, which deserve more research and attention. At the very least, we should invest as many obesity research dollars in uncovering and understanding these biological channels as we do in understanding behavioral channels. And this is a behavioral economist talking!
After all, this could radically change the way we think about policies to curb obesity. As one newspaper editorial pronounced:
“A little town in Sweden has put a local tax on fat men. It is declared that ‘the fat man stands accused by the very fact of his too solid flesh’ (vide “Hamlet”) ‘of gluttony and laziness.’ Millions of fat men throughout the world may rise up and denounce as liars the town councillor who drew up this cruel indictment and those who voted for it, but the gentler way of reproving them would be to point out the tritely recognised danger of generalisation in almost any statement of supposed fact. Not all fat men are lazy and gluttonous. Obesity is in many a congenital habit of body; in others a disease.”
That editorial was written in 1923, for the paper known as The Paris Herald. Maybe the writer was on to something.
SENDHIL MULLAINATHAN is a professor of economics at Harvard.
This article has been revised to reflect the following correction:
Correction: November 17, 2013
Because of an editing error, the Economic View column last Sunday, about possible causes of obesity, misstated the source of bacteria that were transplanted into mice as part of an obesity study. The bacteria came from human twins, not from other mice.
A version of this article appears in print on November 10, 2013, on page BU6 of the New York edition with the headline: The Co-Villains Behind Obesity’s Rise.
Preventing medical error
- diagnostic errors are the most preventable medical mistakes
- Automation is part of the solution – sifting through medical records to look for potential bad calls, or to prompt doctors to follow up on red-flag test results.
- Another component is devices and tests that help doctors identify diseases and conditions more accurately
- online services that give doctors suggestions when they aren’t sure what they’re dealing with
- changing medical culture is another approach
Source: http://online.wsj.com/news/articles/SB10001424052702304402104579151232421802264
The Biggest Mistake Doctors Make
Misdiagnoses are harmful and costly. But they’re often preventable
Such devastating errors lead to permanent damage or death for as many as 160,000 patients each year, according to researchers at Johns Hopkins University. Not only are diagnostic problems more common than other medical mistakes—and more likely to harm patients—but they’re also the leading cause of malpractice claims, accounting for 35% of nearly $39 billion in payouts in the U.S. from 1986 to 2010, measured in 2011 dollars, according to Johns Hopkins.
The good news is that diagnostic errors are more likely to be preventable than other medical mistakes. And now health-care providers are turning to a number of innovative strategies to fix the complex web of errors, biases and oversights that stymie the quest for the right diagnosis.
Part of the solution is automation—using computers to sift through medical records to look for potential bad calls, or to prompt doctors to follow up on red-flag test results. Another component is devices and tests that help doctors identify diseases and conditions more accurately, and online services that give doctors suggestions when they aren’t sure what they’re dealing with.
Finally, there’s a push to change the very culture of medicine. Doctors are being trained not to latch onto one diagnosis and stick with it no matter what. Instead, they’re being taught to keep an open mind when confronted with conflicting evidence and opinion.
“Diagnostic error is probably the biggest patient-safety issue we face in health care, and it is finally getting on the radar of the patient quality and safety movement,” says Mark Graber, a longtime Veterans Administration physician and a fellow at the nonprofit research group RTI International.
Big Efforts Under Way
The effort will get a big boost under the new health-care law, which requires multiple providers to coordinate care—and help prevent key information like test results from slipping through the cracks and make sure that patients follow through with referrals to specialists.
There are other large-scale efforts in the works. The Institute of Medicine, a federal advisory body, has agreed to undertake a $1 million study of the impact of diagnostic errors on health care in the U.S.
In addition, the Society to Improve Diagnosis in Medicine, which Dr. Graber founded two years ago, is working with health-care accreditation groups and safety organizations to develop methods to identify and measure diagnostic errors, which often aren’t revealed unless there is a lawsuit. In addition, it’s developing a medical-school curriculum to help trainees improve diagnostic skills and assess their competency.

Robert Wachter, associate chairman of the department of medicine at the University of California, San Francisco, says defining and measuring diagnostic errors is an important step. “Right now, none of the incentives for improvement in health care are based on whether the doctor made the correct diagnosis,” Dr. Wachter says. But equally important, he adds, “we need to nurture bottom-up innovation.”
That’s already happening. Large health-care systems are mining their electronic records for missed signals. At the Southern California Permanente Medical Group, part of managed-care giant Kaiser Permanente, a “Safety Net” program periodically surveys its database of 3.6 million members to catch lab results and other data that might fall through the cracks.
In one of the first uses of the system, a case manager reviewed 8,076 patients with abnormal PSA test results for prostate cancer, and more than 2,200 patients had follow-up biopsies. From 2006 to 2009, 745 cancers were diagnosed among those patients—and Kaiser had no malpractice claims related to missed PSA tests.
The program is also being used to find patients with undiagnosed kidney disease, which is often found via an abnormal test result for creatinine, which should be repeated within 90 days. From 2007 to 2012, the system found 7,218 lab orders placed for patients with an abnormal test that had not been repeated. Of those, 3,465 were repeated within 90 days of a notice to patients that they needed a repeat test, and 1,768 showed abnormal results. The majority, 1,624, turned out to be new cases of the disease.
Michael Kanter, regional medical director of quality and clinical analysis, says the system enables clinicians to go back “as far as is feasible to find all of the errors that we can and fix them.”
Because the disease is slow moving, Dr. Kanter says, people with a five-year-old undiagnosed case may not have been harmed. Likewise, with many early prostate cancers, “in many of these cases it doesn’t mean harm would have reached the patient,” he says. “But we don’t want patients not to have the information they should have had through some kind of lapse in the system.”
Dealing With the Flood
Electronic records aren’t a panacea, of course, and can even lead to information overload. In a survey of Veterans Administration primary-care practitioners reported last March in JAMA Internal Medicine, more than two-thirds reported receiving more patient-care-related alerts than they could effectively manage—making it possible for them to miss abnormal test results.
Some researchers suggest the best solution isn’t to flood doctors with information but to provide a second set of eyes to find things they may have missed.
The focus now is preventing dangerous delays in follow-ups of abnormal test results. In a pilot program, researchers at the Houston VA developed “trigger” queries—a set of rules—to electronically identify medical records of patients with potential delays in prostate and colorectal cancer evaluation and diagnosis. Records included charts that had no documented follow-up for abnormal findings suspicious for cancer after a certain period, according to the research team’s leader, Hardeep Singh, chief of health policy and quality at Michael E. DeBakey VA Medical Center in Houston and an assistant professor of medicine at Baylor College of Medicine.
The queries were run on nearly 600,000 records of patients seen at one VA facility in 2009 and 2010. Dr. Singh says the use of triggers, which helped find abnormal PSA tests and positive fecal occult blood tests, could detect an estimated 1,048 instances of delayed or missed follow-up of abnormal findings annually and 47 high-grade cancers.
The VA has funded a randomized trial to test whether an automated surveillance system of triggers can improve timely diagnosis and follow-up for five common cancers.
“This program is like finding needles in a haystack, and we use information technology to make the haystack smaller and smaller so it’s easier to find the needles,” Dr. Singh says.
More health-care systems are also turning to electronic decision-support programs that help doctors rank possible diagnoses by likelihood based on symptoms and notes in the medical record. In a study of one such system, called Isabel, researchers led by Dr. Graber found that it provided the correct diagnosis 96% of the time when key clinical features from 50 challenging cases reported in the New England Journal of Medicine were entered into the system. The American Board of Internal Medicine is studying how Isabel could be linked to assessments of physician skill and knowledge.
Another system, DXplain, developed at Massachusetts General Hospital in Boston, was shown in a study last year to significantly improve diagnostic accuracy among first-year medical residents.
Edward Hoffer, associate clinical professor at Harvard and senior computer scientist at Mass General who leads the DXplain program, says the aim now is to have DXplain “push” diagnostic suggestions to physicians through an electronic-medical-records system rather than requiring doctors to initiate a query, which some are still reluctant to do. “We have to focus our attention on dealing with situations where doctors think they know what the diagnosis is, but they don’t,” Dr. Hoffer says.
Other Avenues
New devices also hold promise for confirming a diagnosis and avoiding unnecessary tests. A number of companies are rushing to provide aids such as portable diagnostic equipment and lab tests that can analyze tiny samples of blood and other bodily fluids quickly to detect disease.
Consider MelaFind, which came to market in the U.S. in 2011. The device allows dermatologists to noninvasively examine moles as deep as 2.5 millimeters beneath the surface to gauge the level of “disorganization,” an indicator of irregular growth patterns that are a sign of melanoma, among the deadliest cancers.
New York dermatologist Macrene Alexiades-Armenakas says she uses MelaFind to confirm that a mole is to be removed and prioritize the level of disorganization in multiple abnormal moles. In some cases, when another doctor or the patient has been concerned about a mole, MelaFind supported “clinical diagnosis of a benign mole, thereby sparing them a biopsy,” she says.
But such devices will never replace a thorough physical exam with a trained eye and careful follow-up, says Dr. Alexiades-Armenakas: “These diagnostic tools are aids to increase our accuracy and adjuncts to good physical diagnosis, not a substitute.”
Some efforts to cut down on errors take a different route altogether—and try to improve diagnoses by improving communication.
For instance, there’s a push to get patients more engaged in the diagnostic process, by encouraging them to speak up about their symptoms and ask the doctor, “What else could this be?” At Kaiser Permanente, a pilot program provides patients with a pamphlet that encourages them to think about and write down their symptoms and what concerns or fears they have, encouraging them to ask specific questions to be sure they understand their diagnosis and the next steps they must take.
Medical schools, meanwhile, are teaching doctors to be more receptive to patient input and avoid “anchoring,” the habit of focusing on one diagnosis and excluding other possible scenarios, and “premature closure,” not even considering the correct diagnosis as a possibility.
The Critical Thinking program at Dalhousie University in Halifax, Nova Scotia, established last year, aims to help trainees step back and examine how biases may affect their thinking. Developed by Pat Croskerry, a physician known for his research on the role of cognitive error in diagnosis, it uses a list of 50 different types of bias that may lead to diagnostic error.
The program is being integrated throughout four years of the medical school. Students study cases such as a psychiatric patient with shortness of breath who was assumed to be merely having an anxiety attack; doctors overlooked that she was a smoker on birth-control pills, a risk for the blood clot that later traveled to her lung and killed her.
“If we can teach physicians how to think more critically,” Dr. Croskerry says, “they would be more effective in delivering good care and arriving at the right diagnosis.”
Ms. Landro is an assistant managing editor for The Wall Street Journal and writes the paper’s Informed Patient column. She can be reached at laura.landro@wsj.com.
fat getting fatter
- eat less and exercise more
- Jim Clifton is Chairman and CEO of Gallup
America’s Biggest Fiscal Problem: The Fat Are Getting Fatter
 Much of U.S. politics focuses on the fact that the rich are getting richer and the poor, poorer. But does anyone care that the fat are getting fatter?
Much of U.S. politics focuses on the fact that the rich are getting richer and the poor, poorer. But does anyone care that the fat are getting fatter?
The U.S. adult obesity rate so far this year is on pace to surpass all annual average obesity rates since Gallup-Healthways began tracking it five years ago.
Health costs are going to bankrupt us. At the current annual 6% growth rate, our total healthcare bill will go from $2.5 trillion per year — which it is now — to almost exactly $4.5 trillion in 10 years. If you add the stubs of the increases over the 10-year period, above the running $2.5 trillion our debt-burdened nation can’t afford, it totals a staggering $10 trillion.
To put this in perspective, the sum of our coming healthcare costs are three times the size of the subprime meltdown that brought America and the world to its knees. While we survived the subprime mess, healthcare costs will honestly break the nation.
Things look even worse when you compare America’s per person healthcare spending to comparable societies. We spend more than $8,000 annually per person, where Canada and Germany each spends roughly $4,500 per person, and the United Kingdom spends about $3,500, according to the Organisation for Economic Co-Operation and Development — and residents of those countries all live longer.
So is our American healthcare system superior? You tell me.
Americans obviously understand that this is a huge problem. Nearly a quarter of us say cost is the most urgent health problem facing the U.S., surpassing healthcare access for the first time since 2006. Obesity remains the No. 1 health condition named.
Keep in mind that all of the hoopla about the Affordable Care Act (ACA), or Obamacare, has little to do with reducing the bloated and growing $2.5 trillion expense. Obamacare attempts to address the insurance issue — who pays for what — but it doesn’t go after the core problem: Americans are too fat and unhealthy, and the vast majority of our health problems arepreventable.
That’s right — the Centers for Disease Control concluded a few years ago that of all of America’s chronic health problems, a whopping 70%, are preventable. And what is the common thread among these chronic diseases, such as diabetes and heart disease? Being obese puts people at higher risk for developing all of them.
Rather than go on and on about whether the ACA website works or not, or who wins and loses politically in 2014 and 2016 because of a disastrous rollout, shouldn’t the media be trumpeting this headline: 70% of Health Problems in America Are Preventable?
I just figured the overall weight of Americans, and it’s right at about 56 billion pounds if I assume 180 pounds per person. As a nation, in my view if we collectively lost about 10 billion pounds of excess weight, we might reduce our healthcare costs by a third. And we wouldn’t need all of these wasted political conversations, because we could balance the budget. Even better, the fix would be free — it wouldn’t require a new law, sequestration, or a shutdown.
That’s because the real fix doesn’t lie within political battles over insurance coverage. It lies within a sudden new culture of American fitness — and that begins with eating less and exercising more.
*****
Jim Clifton is Chairman and CEO of Gallup. He is author of The Coming Jobs War (Gallup Press, 2011).
Katz: lifestyle = breakthrough medical cure = lifestyle = medicine
Lifestyle as Medicine: At a Fork in the Road, Who’s Got a Spoon?
Hippocrates recognized the power of lifestyle as medicine some 2500 years ago, testimony to his wisdom and prescience. As president-elect of the American College of Lifestyle Medicine, I celebrate the possibility of finding our way back to a future informed by such insight.
But for now, in the immediate aftermath of announcement, and on-going debate about just how many of us should take statins, let’s consider what Big Pharma would have to do to compete on an even playing field with the power of lifestyle.
Imagine, for instance, if the news were to break tomorrow – on the landing page of your favorite site, or front page above the paper crease for you traditionalists, in whatever news source you like best – that there is a new prescription drug. The drug is stunningly effective, and shockingly free of side effects. It is astoundingly safe – safe enough for newborns and octogenarians alike. It is available in bountiful supply, and remarkably inexpensive. In fact, you might be able to get it without spending any extra money at all – maybe even save money by taking it.
And, here’s the punch line. If you take this pill – which everyone else in your family can take along with you – once daily for the rest of your life, it would reduce your risk of EVER getting ANY major chronic disease – heart disease, cancer, stroke, diabetes, dementia, etc. – by 80%.
The only question here is which would be a better idea and the more immediate priority: calling your doctor to get a prescription for this wonder drug, or calling your broker to get some share of stock in the company holding the patent.
But, of course, there is no such drug. There never has been any such drug. And in my opinion, there never will be any such drug. But lifestyle is exactly that medicine, and we have known about it …well, since Hippocrates.
But we know about the power of lifestyle as medicine in the modern age in ways unavailable to Hippocrates. A seminal epidemiologic study published in 1993 in the Journal of the American Medical Association famously pointed out that the leading, actual causes of premature death in the United States are not heart disease, cancer, and so on – but the things that cause heart disease, cancer, and so on. Those factors sum up to a list of ten exposureswe each, overwhelmingly have the capacity to control in our daily lives. That list of ten is, in turn, overwhelmingly dominated by just the first three: tobacco use, dietary pattern, and physical activity pattern. Or, as I like to call them – how we use our feet, our forks, and our fingers.
That initial study spawned a whole branch of the epidemiologic literature, reaffirming over a span of decades now that lifestyle is by far the best medicine ever conceived – or, if neglected, a source of years lost from life, and life lost from years. Study, after study, afterstudy, after study, after study…has shown that feet, forks, and fingers are nothing less than the master levers of medical destiny. Add to these three the management of sleep, stress levels, and loving relationships in our lives, and the control over our medical destinies is astounding.
And, in tandem with the literature showing how these factors overmaster our fate with regard to chronic disease risk, there is a burgeoning literature showing that they have the capacity toalter gene expression, too. The Genomic Age has served up a powerful insight, albeit not the one we were expecting: DNA is not destiny. To a greater extent, dinner is destiny – because dinner, and lifestyle, can alter the behavior of our very genes. The nature/nurture debate is rather an unfortunate distraction, because we can, in fact, nurture nature.
Lifestyle is then, irrefutably, the greatest of all medicine. But as we learned from Mary Poppinsif not elsewhere, there is the separate challenge of getting the medicine to go down. Certainlythe last thing we need in this case is more spoons full of sugar!
Lifestyle is the greatest of all medicine, but it may feel in this morbidigenic, obesigenic world of ours that we can’t get it to go down, because we just don’t have the right spoon. It may feel that we can’t get there from here.
That is, in a word, wrong. We can get there from here.
Doing so begins by embracing the destination – by acknowledging that lifestyle is medicine we all want. Then, we have to acknowledge that we do indeed know just what destination we mean, that we know what healthy living looks like. We do – including diet – and if we could get past the distractions of competing dogma, we would have the destination clearly in our sights. I have written extensively about that destination before, in columns, peer-reviewed papers, and textbooks– so if you want more on the topic, just follow the links.
Finally, once the destination is clear – it’s a matter of following a route that leads there. And so we come to it: a fork in the road, where for far too long, a luminous opportunity for better health, and consequently better lives, has languished. A fork where health could remain alongthe road not taken, or find itself on a path of much lesser resistance. It’s time to choose.
Along one tine of our fork is perpetuation of the status quo, where we lose loved ones we don’t need to lose, long before their time. Or perhaps they lose us. It’s a road where we succumb to unnecessary miseries and lose both years from life, and life from years. And where we bequeath the same and even worse to our children – where they inherit along with our abdication an ever greater burden of chronic disease and premature death, at ever younger age. I think, and hope, this road is readily rejected.
Along another tine is a world that makes health more accessible, a better world. My career is devoted mostly to creating such a world. But it’s a long, slow, arduous process. This tine doesn’t lead to any immediate opportunity for each of us. Along this tine, some of us keep working, while the rest of us just keep on waiting on the world to change. It may happen, but I wouldn’t hold your breath.
And then there is the third tine, which leads promptly and without detour to the skill set we need to be the health we want to see for ourselves. It leads us to be the health we want to see for those we love. And of course, when enough of us have changed ourselves, it leads us tobe the changes we want to see in the world as well.
There is a place, an important place even, for lifestyle IN medicine – where health care professionals offer valuable guidance, and counseling that is both constructive and compassionate. But the power of this cannot compare to that of lifestyle AS medicine, where each of us pulls on the master levers of medical destiny every day. Think about the Blue Zones, those places around the world where people live the longest, healthiest, most vital lives. Those benefits are attributed to how they live and to their culture, not to the counseling they get from doctors. We are in control of how we live, if latently. We are in control of our culture-which begins at the level of household, where family values take hold. The cultivation of vitality could be a family value.
You can prescribe yourself lifestyle as medicine. You are the doctor in this case, for yourself and those you love. But as with all doctoring, it requires a skill set. If you don’t have it, you can get it. And frankly, there is no real alternative. No other medicine can do what lifestyle can do, and no one else can practice lifestyle for you. It’s your life, and only you can live it. If you empower yourself- if you acquire the requisite “skillpower” to take lifestyle as your medicine- it will almost certainly be a better life. Healthy people have more fun.
Lifestyle is the best medicine there is, ever was, and likely ever will be. At a fork in the road forhealth care, our economy, our culture, and what the future holds for our children and grandchildren- each of us holds the spoon that could get this medicine to go down.