Plenty of sensible lines, though nothing about fasting…
http://bigthink.com/experts-corner/why-dieting-is-the-worst-way-to-lose-weight
Why Dieting is the Worst Way to Lose Weight
by TOM VENUTO NOVEMBER 23, 2013, 6:00 AM
Dieting is the worst way to lose weight. Most people would say I’m crazy for making such an outrageous claim. However, by the time you finish reading this short article, I think you’ll agree with me: Not only that, my hope is that you’ll agree so much that you’ll join me on my mission against “dieting” — at least the way the multi-billion dollar weight loss industry has been pushing it on everyone for years.
So what on Earth am I talking about, “dissing” dieting like that? Haven’t I said it myself many times before that diet is the most important factor for burning fat and keeping it off? Actually, no. That’s where the misunderstanding is. What I’ve said is that if I were to put the many elements of successful fat loss into the order of their priority, nutrition would be at the top of the list.
There’s a big difference between “diet” and “nutrition”
You may see where I’m going with this now, but you also might be wondering if this is just semantics. Yes, it is. But that’s precisely why “diet” and “nutrition” are not saying the same thing. Words are loaded with meaning between the lines. Being successful is about understanding the power of words — and using the words that successful people use.
Few words are more semantically loaded than diet. Think about what connotations — and whether they are positive or negative. What comes up when you think of diet?
Restriction
Forbidden foods
Banned food groups
What you can “never eat”
Hunger
Gimmicks
Fads/trends (that pass or come and go in cycles)
Quick fixes (often unhealthy or dangerous)
The word “diet” was supposed to simply describe the way a person eats. “Diet” comes from the Latin, diaeta, meaning “way of life.” But in our technologically advanced, sedentary society today, and with the obesity crisis we’re facing, and the multi-billion dollar industry it has spawned, the word “diet” has become tainted . . .
Today, I think ‘diet’ carries too much negative baggage to use so loosely. The way I define it, a diet is any unsustainable change in your eating behavior to try to lose weight. When you say you’re going on a diet, you’re also saying that at some point you’re going off it. While you’re on it, you suffer all those negative associations I mentioned above.
By contrast, think about the connotations of the word nutrition. Do you think of anything negative? I don’t. I think of:
Vitamins
Minerals
Micronutrients
Fiber
Muscle-building protein (amino acids)
Unrefined foods, closer to their form in nature
Energy
Vitality
Health
Now think of the word program. A program implies that there is structure. So I define a nutrition program as a structured plan you can follow as a lifestyle, which nourishes you with nutritious food that helps you get leaner, stronger, fitter and healthier . . . and stay that way.
I propose we replace “diet” with “nutrition program” unless we are specifically talking about something short term.
I believe this distinction in words is crucial, but just to play devil’s advocate, let’s assume that diet and nutrition program mean exactly the same thing. There’s still a huge problem with the diet alone approach, and therefore, why 99% of the entire weight loss industry is wrong:
Diet is only one of the elements needed for a leaner, stronger, fitter, and healthier body. There are three other elements that most people are missing.
Dieting might improve your health. On the other hand, depending on your approach to “diet,” it might destroy your health. Dieting is not always healthy. Nutrition and training together is a sure-fire pathway to health.
Weight loss diets fail 80-95% of the time. Not because they don’t take the weight off, but because they rarely keep it off. Most dieters relapse. Drug addicts and alcoholics in rehab have a higher success rate than that.
Exercise and an active lifestyle are vital for long term weight loss maintenance.
The right kind of exercise is also vital for re-shaping your body . . .
Weight Loss Versus Body Transformation
There’s a world of difference between losing weight and transforming your body.
Dieting can’t transform your body. Only training can do that.
Dieting can’t make you stronger. Only training can do that.
Dieting can’t make you fitter. Only training can do that.
With diets, you might fit into smaller clothes. But you also may become a smaller version of your old self… a skinny fat person . . . weighing less . . . but still flabby (and weak).
The Muscle Loss Epidemic
With diet alone, 30 to 50% of your weight loss could come from lean body mass. And if you’re getting older, the prospect of losing muscle and strength should genuinely frighten you.
After age 50, you lose 1-2% of your lean muscle every year if you do nothing (if you’re not resistance training). After age 60, you lose up to 3% per year.
Let’s suppose you’re 50 or 60 and you’re thinking, “A few percent of my lean mass? What’s the big deal? I have no desire to look muscly.” I can understand that. Your goals and values do change as you get older. But I already realize that most people don’t want to look like bodybuilders. However, gaining lean muscle, strength and fitness will improve the quality of anyone’s life.
Maintaining the muscle you have must be a priority for everyone because losing lean mass every year means losing your mobility and losing your independence as you get older.
Stop the Diet Insanity!
Given these facts, it’s sheer insanity that we have millions of people who want to lose weight — for health and for happiness — and the first thing or only thing they think of as a solution is DIET. They’re asking for deprivation, hunger, missing out on favorite foods, loss of muscle, loss of strength and eventually, loss of independence, putting a burden on other people to take care of them.
I’m not being melodramatic. I’m on mission to expose the mistakes of the dieting mentality and promote the benefits of the muscle-building, fitness and nutrition lifestyle.
The good news is, there’s a right way to burn fat and transform your body, but it’s not a one-trick show. You have to put several pieces together. This is total lifestyle change, so it’s not easy. But it is worth it.
This is as near to a miracle formula as you will ever find. It’s the 4 elements of the Burn the Fat, Feed the Muscle approach:
Nutrition program
Resistance (strength) training
Cardio Training
Mental training
Dieting is the worst way to lose weight
Not only that, here’s the nail in the coffin for 99% of what the weight loss industry is telling you: weight loss is the wrong goal to begin with. Burning the fat and keeping the muscle is the right goal. Even better, the right goal is to get leaner, stronger, fitter and healthier.
Train hard, and expect success.
© 2013 Tom Venuto, author of Burn the Fat, Feed the Muscle: Transform Your Body Forever Using the Secrets of the Leanest People in the World
Author Bio
Tom Venuto is a fat-loss expert, transformation coach and bestselling author of Burn the Fat, Feed the Muscle. Tom holds a degree in exercise science and has worked in the fitness industry since 1989, including fourteen years as a personal trainer. He promotes natural, healthy strategies for burning fat and building muscle, and as a lifetime steroid-free bodybuilder, he’s been there and done it himself. Tom blends the latest science with a realistic, commonsense approach to transforming your body and maintaining your perfect weight for life.
For more information please visit http://www.burnthefatblog.com/ and http://www.burnthefatfeedthemuscle.com/ and follow the author on Facebook and Twitter

 Paul Tarini, team leader for the
Paul Tarini, team leader for the 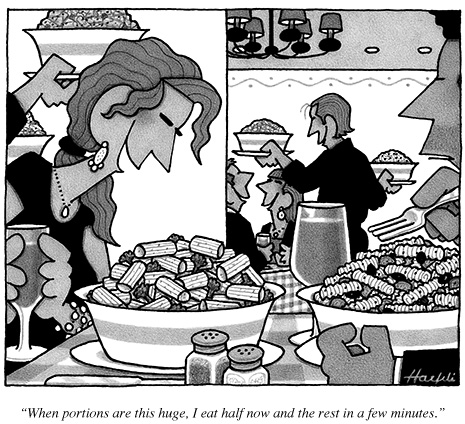
 Daily text messaging may be a useful self-monitoring tool for weight control, particularly among racial/ethnic minority populations most in need of intervention, according to Duke University study results published in a Journal of Medical Internet Research
Daily text messaging may be a useful self-monitoring tool for weight control, particularly among racial/ethnic minority populations most in need of intervention, according to Duke University study results published in a Journal of Medical Internet Research 
 Much of U.S. politics focuses on the fact that the rich are getting richer and the poor, poorer. But does anyone care that the fat are getting fatter?
Much of U.S. politics focuses on the fact that the rich are getting richer and the poor, poorer. But does anyone care that the fat are getting fatter?