http://harvardpublichealthreview.org/the-key-to-changing-individual-health-behaviors-change-the-environments-that-give-rise-to-them/
The Key to Changing Individual Health Behaviors: Change the Environments That Give Rise to Them
PDF: HPHRv2-Stulberg
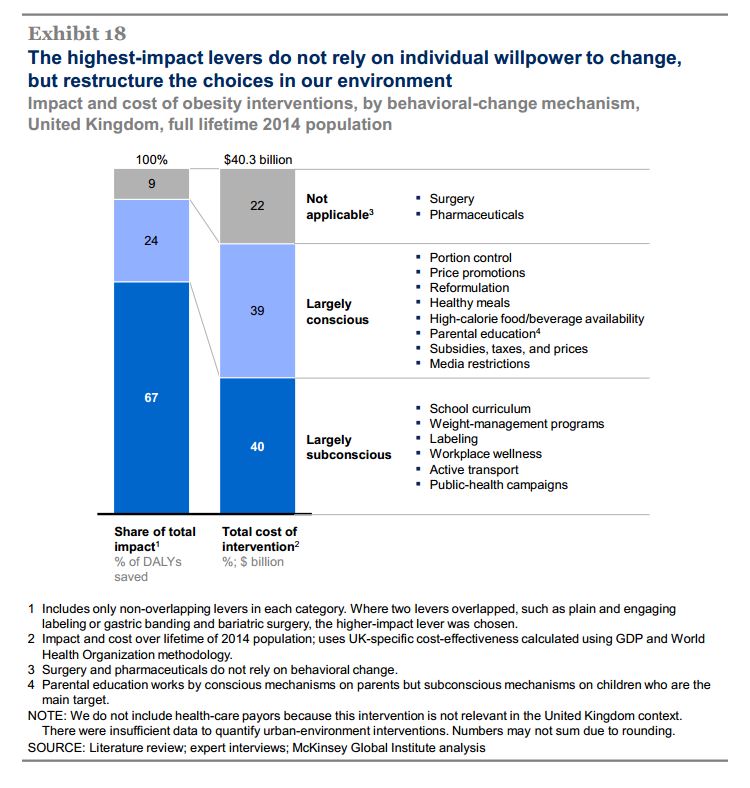
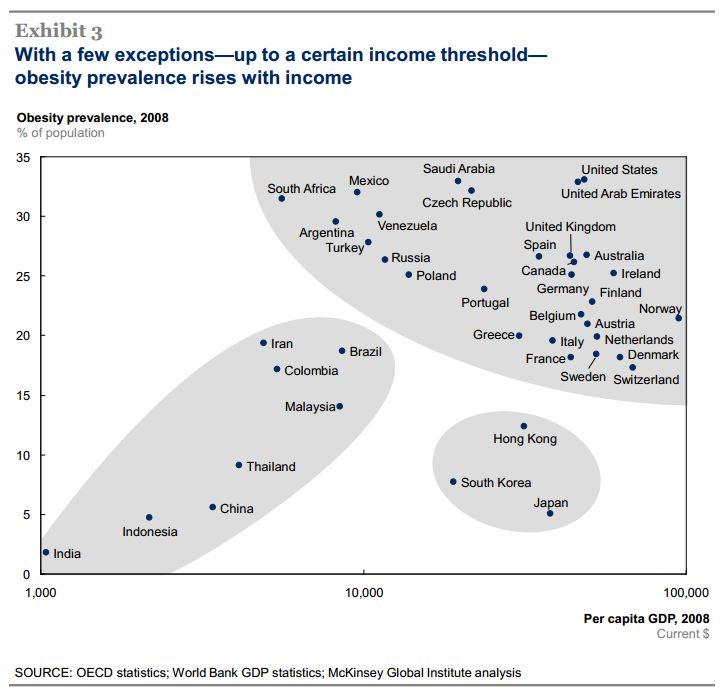
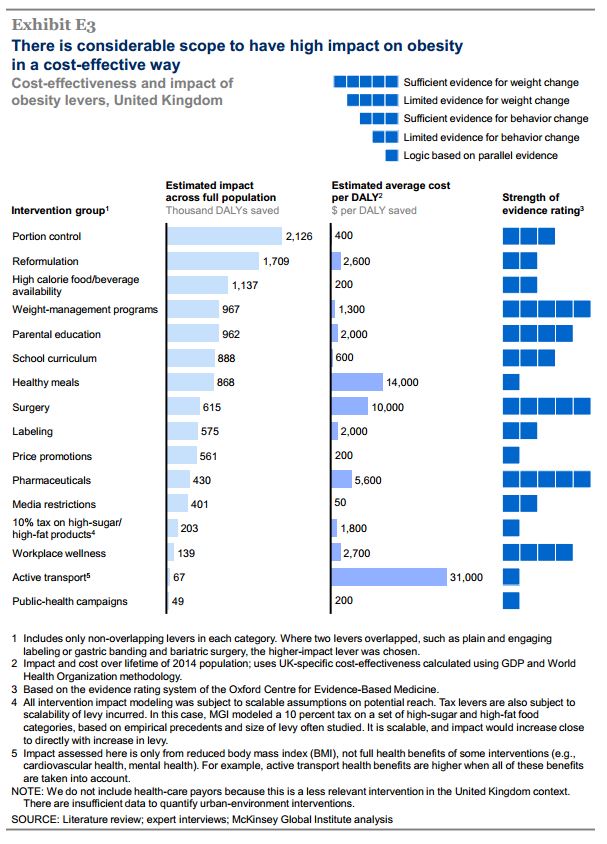
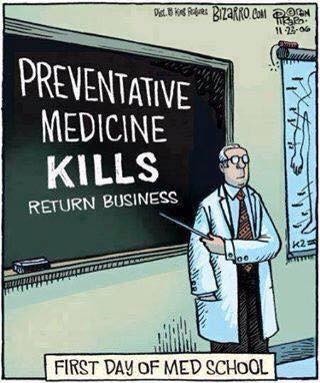
Over the past four decades, the United States has faced steadily rising rates of obesity and associated chronic conditions. Many of these chronic conditions are rooted in nutrition and physical activity behaviors, and are often referred to as lifestyle diseases. Historically, the prevention of lifestyle diseases has focused on changes in individual behavior and personal choices, and personal responsibilities. However, a growing body of research has demonstrated the strong influence of physical and social surroundings on individuals’ actions. The context in which options are presented can shape the decision-making processes that impact health. Altogether, the research suggests that altering environments may be an effective driver of behavior change. Intentionally designing environments to promote healthy behaviors holds promise to reverse the increase of lifestyle diseases.
The emerging field of behavioral science – which gathers insights from disciplines like behavioral economics, cognitive psychology, and social psychology – illustrates that while individuals retain “free choice,” their environment significantly influences the choices they make, and in some instances, may lead them to act in ways that are counter to their true preferences. A few examples:
- Individual preferences are often inconsistent over time, especially in situations where immediate pleasures carry long term consequences. In a study that asked [hypothetically] if people would prefer fruit or chocolate as a future snack, 74% chose fruit. But, when those same participants were presented with both fruit and chocolate in real-time, 70% selected chocolate.
- A person’s actions can be dramatically influenced by related contextual features. For instance, research shows that kitchenware size significantly influences serving and eating behavior. In a series of studies, individuals who were given larger bowls served themselves between 28-32% more cereal than those given smaller bowls. Studies also report that people tend to eat 90-97% of what is on their plate, irrespective of plate size.
- People tend to consent to the “default option.” This has been observed in numerous situations ranging from deciding whether or not to become an organ donor to making saving allocations for retirement. For example, organ donation rates are 4% in Denmark and 12% in Germany where the default option is “opt-in.” In contrast, the rates are 86% in Sweden and nearly 100% in Austria where the default option is “opt-out.” Cultural differences cannot explain the discrepancy.
When these behavioral science insights are applied in the context of health, the growth of lifestyle diseases is not surprising. This expanding body of research sheds light on the difficulties of healthy living when society is dominated by the marketing of unhealthy foods and unduly large portion sizes, and where sedentary behavior is often the default option.
The good news is that the same forces that currently promote unhealthy behaviors can be used to encourage healthy ones. In their bestselling book Nudge, Richard Thaler and Cass Sunstein described “choice architecture,” or the proactive designing of environments that “nudge” people to make healthier selections while still retaining freedom of choice. There are many opportunities to apply this concept to promoting healthy behaviors. In particular, given their resources, broad reach, and financial and social incentives, both governments and employers are in a unique position to promote healthy behaviors in a way that would affect many lives.
Government food programs such as the Supplemental Nutrition Assistance Program (“SNAP”) and the school lunch program could be designed to make healthy selections more accessible, and in some cases, the default options. Those that oppose the trend toward encouraging healthier foods often cite added costs and waste, arguing that children don’t like healthy foods and will throw them away uneaten. But the data tell a different story. A recent study in Childhood Obesity found that a vast majority of middle-school and high-school students like the updated and significantly healthier school lunch that was introduced in 2012.
Nonetheless, making the change is not cost-free. A recent meta-analysis found that the healthiest diets cost $1.50 more per-person, per-day, which amounts to $550 per-person, per-year. While this amount is not insignificant, it pales in comparison to the cost of treating most diet-related chronic conditions. Designing government food programs around the “healthiest diets” may yield a positive return on investment.
Even so, many individuals – including those who do qualify for SNAP, as well as those who do not qualify for SNAP (i.e. incomes just about the SNAP cut-off) – may still struggle with affordability and availability of healthy foods. Perhaps the most sustainable and far-reaching approach to making healthy foods more accessible is to change food policies (e.g., subsidies) that currently favor the production and systematic delivery of unhealthy foods to favor healthy ones. This would likely lead to higher volumes, more efficient delivery, and lower costs for nutritious foods.
The government can also promote healthier eating by improving nutrition labeling. While the FDA’s recent proposal to ensure that serving sizes listed on food products reflect actual average consumption (e.g., nutrition specifications would reflect an entire muffin, not one-third of a muffin) is a small step in the right direction, there is potential to go a lot further. Research suggests that catchier and simplified nutrition labels could have a much greater impact on consumer behavior. For example, NuVal, an independently designed system that gives food items a single overall score based on more than 30 nutrient and nutrition factors, could be considered for more widespread adoption. Not only does NuVal make for easier interpretation of a product’s nutrition profile, it also enables comparison shopping between options and encourages people to “trade-up” to healthier options. An additional model to consider is a traffic-light rating system that marks foods with either a green, yellow, or red light. In instances where it has already been implemented (in some private organizations and outside the United States), the traffic-light model has increased consumer awareness of health and leads to healthier purchases.
In addition to promoting a healthy diet, government should play an active role in encouraging physical activity through the education system (e.g., ensure the existence of meaningful recess and gym programs), transportation system (e.g., create options for safe pedestrian/bike commuting), and by supporting relevant community resources (e.g., building, maintaining, and ensuring the safety of outdoor parks and recreation centers). When options for physical activity are easily accessible, people tend to be more active. For example, a recent study published in the American Journal of Public Health illustrated that the establishment of traffic-free cycling and walking routes increased overall physical activity among those that lived nearby.
Employers may have the ability and incentives to move faster than government in designing health promoting environments. A healthier workforce results in both reduced health care costs and absenteeism, and in increased productivity. Recent data from the Society of Human Resource Management’s annual Employee Benefits Survey shows that employers are taking notice and increasing their investment in workforce wellness programs. While these programs have traditionally focused on offering employees classes, counseling, and incentives for healthy behaviors such as discounts on insurance premiums, subtler tweaks to the workplace itself could prove just as, if not more effective.
An example of these subtler changes is happening at Google. There, company leaders have invested in promoting employee nutrition and health. Instead of relying solely on traditional programs such as nutrition counseling and weight-loss classes, Google redesigned cafeterias to encourage healthier eating. Now, the most nutritious options are positioned at the front of the cafeteria and unhealthy foods are hidden in corners and placed in opaque bowls. Smaller plates are the norm and marked with reminder messages that “bigger dishes prompt people to eat more.” Foods are tagged with either red “warning” stickers, or green stickers signifying healthy foods. Beverage coolers stock water at eye level, and relegate sweetened beverages to the bottom where they are not as easily seen or accessed. These changes – which notably do not restrict options, but simply rearrange the way options are presented – have led to dramatic reductions in candy and sugar-sweetened beverage consumption, and increases in the use of smaller plates.
To encourage physical activity, employers can adopt similar approaches to workplace design, such as centrally located staircases and ergonomically fit workstations. Further, similar to current LEED certifications for environmentally-friendly buildings, there could also be a meaningful certification for health-promoting buildings. In addition to the design of physical workplaces, the way that work itself is conducted can also be designed to promote health. For example, some employers have made “walking meetings” a cultural norm to build physical activity into otherwise sedentary jobs.
Other Considerations
While the value of these environmental interventions is promising, there is a need for additional research that focuses on cost effectiveness. This is especially true if we hope to see increased governmental action, where broad policy implementation almost always follows a positive cost/benefit analysis. That said, some of the ideas – such as using smaller plates in government cafeterias or simplifying nutrition labels – come at relatively little additional financial cost, and have already demonstrated health-promoting benefits. These ideas could be fast-tracked for more widespread adoption.
Another potential barrier that must be overcome is the political power of special interests groups that rely on built-environments conducive to unhealthy behaviors. For example, a large part of the reason that the migration to healthier school lunches has taken so long is because various food interests have launched strong lobbying campaigns against such changes. In order to transition entrenched unhealthy built-environments to healthier ones, policymakers will need to prioritize the demands of public health against the backdrop of influential and longstanding special interests
A broader approach to designing environments that promote healthy behaviors must also account for additional barriers that individuals with lower socioeconomic status commonly face. The government cannot rely solely on the private sector to drive these changes since those who stand to benefit most may be unemployed or not working for progressive employers with the resources to launch effective health campaigns. Thus, focusing on government food programs and community-based approaches that effect a lower-income demographic is critical (e.g., sidewalk coverage and safe streets, eliminating food deserts, maintaining outdoor parks). In addition to these more specific interventions, the clear connection between environment and health should only bolster the case for expanding social service programs more broadly. Realizing and addressing the fact that so many of the outcomes that lie inside of health care are rooted in factors that lie outside of health care is thus critical to improving health.
If we want to avert a public health crisis at the hands of chronic lifestyle-driven diseases, we need not only focus on changing individual behaviors, but also on changing the environments that give rise to those behaviors. Governments and employers must recognize the overwhelming influence of context on action, and take advantage of their unique position to intentionally shape environments that promote healthy behaviors.