- Leading US providers are using analytics to bring a more intense focus on gaps in care, to discover cost outliers, and to put a magnifying glass on efficiency
- “Unlike other industries that may be high users of data and very sophisticated, the healthcare industry is at a different point”
- “A platform where we mesh both claims data and data out of our electronic health records allows a lot more to be learned. The type of intelligence that we can glean is at a much more informed level than if we’re just dealing with one of those data sets in isolation.”
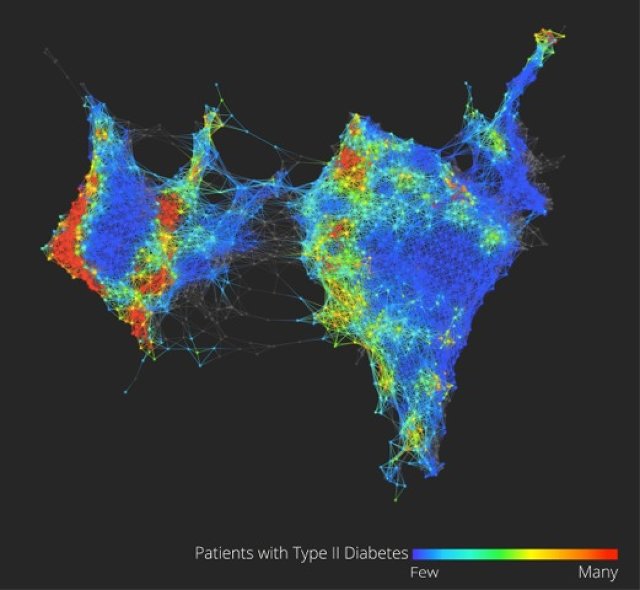
- At the heart of population health analytics is the concept of risk stratification: understanding, through various inputs such as claims data, surveys, and EHRs, which members of a given healthcare organization’s customer base represent a level of risk for which intervention offers the greatest possibility of preventing future hospital admissions, reducing readmissions, improving overall health, and lowering costs.
- Cleveland Clinic’s Explorys pulls data from a variety of sources—multiple electronic health records, billing systems, claims data from CMS and other payers—and assimilates that all together to allow filtering, reporting, identify care gaps and registry functions
- A variety of tools exist to help stratify risk:
> Some tools place members of a population on a scatter plot to make the identification of outliers easier
> Other tools organize a population into patient registries to track various diseases and treatments
> Still other tools use input gathered from patient surveys.
- near-real time data is an important addition
http://www.healthleadersmedia.com/content/TEC-298525/How-Population-Health-Analytics-Opens-Opportunities-for-Better-Care
How Population Health Analytics Opens Opportunities for Better Care
Scott Mace, for HealthLeaders Media , November 20, 2013
Innovators are blending technology with new care models while targeting high-risk patients in a patient-centered strategy.
This article appears in the November issue of HealthLeaders magazine.
Without robust analytics technology, the goals of accountable care and population health cannot fully be achieved, good intentions notwithstanding. ACOs must correlate clinical data and claims data and use analytics technology to produce the actions needed to manage the health of a population. The data is there, but the healthcare industry does not have an evenly distributed knowledge of how to use it effectively.
With potential savings of up to $300 billion a year, according to the consulting firm McKinsey & Company, the upside of industrywide analytics to manage a population is considerable.
And, increasingly, providers have the raw data they need to feed an analytics system. But it is not as simple or quick as installing electronic health record technology—no small feat in itself for many organizations—and must be accompanied by solid governance and education, according to leading providers.
These providers are using analytics to bring a more intense focus on gaps in care, to discover cost outliers, and to put a magnifying glass on efficiency. But the use of such healthcare analytics has yet to reach maturity.
Early in the process
“Our organization is facing what most of the industry is facing, and that is the need to build a bridge to the future through analytics; so unlike some other industries that may be high users of data and very sophisticated, the healthcare industry is just in a different point,” says Aric Sharp, vice president of the accountable care organization at UnityPoint Health, a West Des Moines, Iowa–based integrated health system with 3,026 licensed beds across 15 hospitals and total operating revenue of $2.7 billion.
“We’re still in the process, as an industry, of going through implementing electronic health records and achieving meaningful use and those types of things. At the same time, with a lot of the new efforts around accountable care organizations, for one of the first times many providers have an opportunity to collect claims data by working with payers,” Sharp says. “We felt it necessary to build a platform where we can mesh together both claims data and data out of our electronic health records, because there’s a lot more that’s able to be learned in that type of an environment. The type of intelligence that we can glean is at a much more informed level than if we’re just dealing with one of those data sets in isolation.”
UnityPoint Health typifies numerous providers, having initiated analytics for its population health initiative only a couple of years ago. “The primary lesson is, this is really difficult, and there’s a lot to learn along the way,” Sharp says. “And yet, we can certainly see that as we continue to enhance the work, there’s more and more benefit with every step. The big learning is that there’s just a lot to be learned, and it’s exciting, because with every step of the process, we are better able to identify opportunities to improve care, and we’re able to become more efficient at this type of work.”
At the heart of population health analytics is the concept of risk stratification: understanding, through various inputs such as claims data, surveys, and EHRs, which members of a given healthcare organization’s customer base represent a level of risk for which intervention offers the greatest possibility of preventing future hospital admissions, reducing readmissions, improving overall health, and lowering costs.
UnityPoint Health selected analytics technology from Explorys, a data spinoff of Cleveland Clinic founded in 2009.
“Explorys is able to pull data from a variety of sources—multiple electronic health records, our own billing systems, claims data from CMS or other payers—and assimilate that all together,” Sharp says. “Explorys is really what sits on top of that and gives us an ability to slice and dice and analyze it and probe it and report quality metrics, identify gaps in care, and in the future even use that to do outreach to patients and do registry-type functions.”
UnityPoint Health still counts the time until the big payoff in years. “We’re not yet ready to say that it has an impact on our global per-member per-month spent,” says Vice President of Operations Kathleen Cunningham. “It will, but we are so early in our innovation that some of our results are really based on the pilot type of innovation programs that we’re working on.”
Starting with employee populations
In many healthcare systems, population health analytics success stories are just beginning to emerge, but some providers have used their own employee populations as a proof of concept for the effectiveness of the effort.
For the past 11 years, employees of Adventist HealthCare—a nonprofit network based in Gaithersburg, Md., with three acute care and three specialty hospitals, 6,263 employees, and 2012 revenue of $726 million—have been managed for risk by the self-insured provider.
“It got started with the idea that a healthier population is going to be a more effective employee population, and it’s going to also be a lower-cost population,” says Bill Robertson, president and CEO of Adventist HealthCare.
A decade ago, Adventist started working with InforMed Healthcare Solutions, since acquired by Conifer Health Solutions, to use InforMed’s set of data warehouse tools to improve its health plan design and determine where interventions were needed, Robertson says. Adventist and InforMed worked collaboratively to develop those tools and restructure the Adventist workflow to ramp up the effectiveness of the population health program.
As a result of population analytics, as well as other measures such as discouraging tobacco use and encouraging use of generic drugs, the inflation rate of Adventist’s employee health plan cost over the past nine years was half the national average, Robertson says.
A key development in the population health initiative came in 2005, when Adventist created personal health nurses as part of a pilot patient-centered medical home to work with the approximately 360 high-risk members of Adventist’s 6,600 employee-based covered lives identified by the InforMed data tools, Robertson says.
In a pilot, Adventist selected 27 of 50 high-risk patients (54%) and was able to move them out of the high-risk pool into moderate or low-risk pools, and it achieved a 35% reduction in the cost of care for that population, he says.
According to Adventist, the pilot project that achieved the 35% reduction did reduce health plan costs by $381,000 among the 27 patients who moved from the high-risk pool. The amount expended to achieve this 35% reduction was only $31,000, so every dollar spent returned approximately $12 in savings.
“It was actually so dramatic that it brought the inflation rate on our health plan to zero in that year,” Robertson says. “We were pretty pleased with that.” Overall, Adventist has saved “tens of millions of dollars” due to employee population health analytics to reshape the program and services for employees, he says.
Adventist then expanded this pilot PCMH to 5% of its employees (roughly 360 people), and continues to see the same kind of positive outcomes, Robertson says. Nurses make up the majority of InforMed users.
Three years ago, Adventist created ACES, which stands for Ambulatory Care EHR Support, an initiative to move its ambulatory physicians to use electronic medical records to expand its capacity to do population-focused care. By the end of 2013, more than 400 physicians will be using the ACES system. “So much of the job is how you integrate care across physicians and across the delivery system,” Robertson says. “When you have one person who’s seeing 15 physicians, but each physician thinks they’re the only one, you end up with different challenges than when you can see everything.”
All physicians who are participating providers in the Adventist HealthCare employee health benefit plan have access to the InforMed tools and analytics. Only a limited number directly access the information because the personal health nurses provide most of the ongoing care management, with the physicians serving more as the team captains, Robertson says.
The next step for Adventist IT is to tie analytics with the employee EHR. “What we’re morphing toward is linking all of this together with HIE infrastructure so that the information that is in the InforMed platform will be available in your EHR platform and vice versa through the information exchange,” Robertson says.
Adventist also created financial incentives that help its physicians spend “all the time it takes” to manage high-risk patients, Robertson says. “With an ACO, you don’t really get paid an incentive until you’ve been successful—at least after the first year you’ve demonstrated that things are working and that they’re [generating] shared savings,” he says. “So we’re still in the process of sorting out how we’ll make sure this infrastructure is utilized actively.”
Detailing the financial incentives, Robertson says the primary care physicians who participate in the patient-centered medical homes receive additional compensation, such as a monthly retainer or hourly incentive to compensate them for the additional time that is necessary to care for the high-risk patients in the PCMH.
Recent headlines have highlighted some fallout from the Pioneer ACO program. Fifteen charter members dropped out of the program after finding inadequate return on investment or improvement from their ACO initiative. To Robertson, this just highlights the importance of population health analytics in achieving ACO success. Had Adventist focused on no-risk or low-risk populations, it might not have achieved nearly the cost savings it had with its own proof of concept by targeting the high-risk pool of its self-insured employee-based covered lives, he says.
Now Adventist is forming an ACO for Medicare populations based on this same set of tools to track high-risk members of those populations. As time goes on, commercial-payer populations are also in Adventist’s sights. “We have a couple of pilots, like an apartment building that has a very large population of higher-risk individuals that we’re providing those types of services to, and it’s interesting to see when you focus on it what you achieve in terms of reduced consumption of healthcare services and increased health status,” Robertson says.
Leading the way to better patient care
At Virtua Health, population health analytics from Alere Analytics is being implemented to determine the highest-risk patients from a cohort of 12,000 attributed Medicare lives, says James Gamble, MD, chief medical information officer of the four-hospital, 885-staffed-bed integrated delivery network headquartered in Marlton, N.J.
Virtua became an ACO on January 1 and is preparing to add another 14,000 covered lives with a commercial insurer, says Alfred Campanella, Virtua’s executive vice president of strategic business growth and analytics.
“There are lots of different scenarios where action is needed to prevent an admission or to prevent a condition from getting worse,” Campanella says. Virtua is working with Alere to publish its alert lists via a Microsoft Dynamics customer relationship management platform. “That allows care nurses to take advantage of our Microsoft products like email and word processing,” he adds.
Virtua uses RNs to provide close case management of the high-risk population. Meanwhile, 80 Virtua-employed primary care doctors are kept updated via the workflow into the system’s electronic health record software. “That way that doctor doesn’t have to leave their EMR or jump around to see where things are going,” Campanella says.
“Our initial focus,” Gamble explains, “will be on these high-risk patients, so as we see it, these case managers’ day-to-day job will be: They’ll have a patient load, they will have care plans, they will have activities assigned to them for these patients.”
But the physician does not need to be the primary manager.
“As long as patients are following care plans, which are developed and approved by the providers, then the nurses will be managing them,” Gamble says. “Their communication will be more as updates. When an alert arises that the patient is at risk or in trouble, then obviously the nurse would directly communicate with the physician to try to intervene at any early stage before the patient’s health deteriorates or the patient ends up in the emergency room of the hospital.”
“What we’re seeing now is a more intense focus to try to fix those gaps in care and to identify patients who are at high risk for hospitalization or readmission or who need special attention,” Campanella says. “Technology gives you a greater magnifying glass in many respects for seeing the barriers to care and for creating efficiencies in care delivery. While all the analysis is not complete, early results for clinical and financial savings are promising.”
Support from top leadership has been crucial to Virtua’s transformational pivot toward analytics. “This whole idea of care coordination was approved at the board of trustees level,” Campanella says. “We’ve had tremendous support from our CEO, Richard Miller. One of our senior vice presidents, Stephen Kolesk, MD, doubles as the president of this subsidiary that is the ACO. He has a title of senior vice president for clinical integration, so it’s very tightly integrated with the physicians.”
Technical design of the Virtua analytics solution is close to completion. Parts of it will deploy before the end of 2013, and other parts will roll out in the first quarter of 2014, says Campanella. Also part of the project are an existing health information exchange and a new patient portal built on top of the HIE, he adds.
“Innovation does require some experimentation and risk,” Campanella says. “The ones who are leaders are taking on some risk and putting some investment in without fully understanding the full picture, but that’s what makes them leaders.
“It’s now the right way to care for patients, to have this high touch, high visibility into all the different domains of their care and the handoffs between those domains, and so even if the ACO concept from a regulatory standpoint goes away, it’s still the right way to care for patients,”
Campanella says.
Outside the hospital walls
Organizations beyond postacute hospitals are also engaging healthcare in a variety of ways that have broad implications for how analytics will be deployed in healthcare across the United States.
Brentwood, Tenn.–based Brookdale Senior Living owns and operates about 650 senior living communities in 36 states. In 2012, Brookdale, through a partnership with the University of North Texas Health Science Center and Florida Atlantic University, received $2.8 million of a $7.3 million Centers for Medicare & Medicaid Services Health Innovations Challenge grant for population health management. The program expects to save more than $9 million over a three-year period.
Initially, Brookdale is focusing on population health at 27 communities in Texas and Florida, but by the end of the three-year grant, it will involve 67 communities, says Kevin O’Neil, MD, chief medical officer of the organization.
The CMS grant sets a goal for Brookdale of reducing avoidable hospital readmissions by 11%, O’Neil says. “We know we’re going to be focusing on certain quality metrics in addition to readmissions,” he says. “We’ll focus on dehydration rates, as well as new incidents of pressure ulcers, some of the major problem areas in geriatric care, and then, based on the data that we receive from the analytics tool, it’ll help guide our quality improvement teams in terms of the type of improvement efforts that need to be initiated.”
A variety of tools exist to help stratify risk. Some tools place members of a population on a scatter plot to make the identification of outliers easier. Other tools organize a population into patient registries to track various diseases and treatments. Still other tools use input gathered from patient surveys. A recent study, however, reported that many of those tools had not performed very well.
At St. David’s Health System in Austin, which is working with Brookdale on the challenge grant, 60% of readmissions recently were measured as coming from low-risk groups. “To me [this] means either that people hadn’t been stratified properly, or that they were being sent home when they probably did need some kind of service or follow-up,” O’Neil says.
The biggest hurdle in O’Neil’s experience with population health analytics has been engaging with the hospital C-suite to craft the business associate agreements necessary to manage populations. “Once we’ve developed a relationship with one entity and had success, it’s much easier to engage other entities within that system.”
In dealing with the two universities, O’Neil says, “We had to resolve some issues related to intellectual property to incorporate INTERACT into electronic information systems,” he says. INTERACT is an acronym for Interventions to Reduce Acute Care Transfers, a free quality improvement program for which FAU holds the trademark and copyright. “This has been resolved through a licensing agreement—Loopback [a Dallas-based analytics platform vendor] also has a licensing agreement with FAU to bake INTERACT tools into software programs.”
Both Brookdale and its hospital partners are using a common population health analysis dashboard and software provided by Loopback Analytics. “As a geriatrician, this is the most exciting time in my career, because I’ve always felt that fee-for-service medicine was the bane of good geriatric care because it rewarded volume rather than quality,” O’Neil says. “Having that near-real-time data is really going to be extremely helpful to us.”
Analytics and meaningful use
Analytics tools produce the patient registries that identify gaps in care, not just to meet ACO objectives, but also to meet the requirements of meaningful use stage 2, which takes effect in 2014, says Gregory Spencer, MD, a practicing general internist and chief medical officer at Crystal Run Healthcare, a multispecialty practice with more than 300 physicians based in Middletown, N.Y.
“There are frequently registry functions within EHRs, but the EHR is set up at the patient level,” Spencer says. “It’s not optimized for reporting groups of patients, so to kind of get that rollup, you have to have another layer on top of that to gather it up.”
Thus, some sort of aggregator function is needed. “Usually that is not something that many EMRs do well,” Spencer says. “Registries are mostly condition- or disease-specific lists of patients who satisfy a certain criteria: diabetics, patients with vascular disease, kids with asthma. Care gaps look at all patients who have not had a certain recommended service. There is overlap with the registries, since a list of patients due for their colonoscopy is a kind of registry that needs to be ‘worked’ to get those patients compliant.”
Like numerous other healthcare organizations, Crystal Run’s first foray into population health analytics employed Microsoft Excel spreadsheets.
“The basics can be done with available tools,” Spencer says. “People shouldn’t wait for the killer app that’s out there that’s fancy and has a slick user interface. You can really do a lot with what you have, probably immediately.”
Since 1999, however, Crystal Run has incrementally left Excel behind and built population health analytics reporting tools on top of its NextGen electronic health record software, Spencer says. Crystal Run also adopted the Crimson Population Risk Management service from the Advisory Board Company, which incorporates technology from Milliman Inc. on the back end, he says.
Like other providers, Crystal Run saw the shift coming from fee-for-service to accountable care and took early opportunities to get its hands on claims data and learn how to work with it, Spencer says.
Other resources offering insight to accountable care analytics were the Group Practice Improvement Network and the American Medical Group Association, where Spencer has been able to network with peers who have been pursuing population health analytics longer than Crystal Run has.
The Crystal Run practice, formed in 1996, grew out of a single-specialty oncology practice and today has 1,700 employees. It is designated by the NCQA as a level 3 patient-centered medical home, and in 2012, Crystal Run became one of the first 27 Medicare Shared Savings ACOs.
Analytics have revealed “a lot of surprises at who you think has been getting most of their care from you,” he says. Snowbirds—typically someone from the Northeast, Midwest, or Pacific Northwest who spends substantial time in warmer states during the winter—are receiving significant amounts of care that had been outside of Crystal Run’s knowledge.
But with Medicare claims data examined through its analytics services, Crystal Run has had its eyes opened to previously unobserved cost centers. For instance, the No. 1 biller of pathology services for a 10,000-patient Crystal Run cohort was discovered to be a local dermatologist.
“What it’s all about is improving quality and eliminating waste,” Spencer says. “That waste is [in] tests that aren’t really required [and even some] visits that are [being required]. It’s your habit and custom to see people back at a certain frequency, but when you really start thinking about it, do you really need to see somebody back every three months who has stable blood pressure and has been rock solid? Well, probably not. And so you start doing things like that, and it adds up incrementally.”
Crystal Run is able to incorporate patients’ outside visits to providers, Spencer says, “but it’s not easy. We require source documentation to satisfy measures. For example, we scan outside mammogram results into a directory that we can then report against. We don’t take people’s word for dates. We need to have the document.”
Getting the initial claims data from CMS took three months, and then it takes another three or six months’ worth of that data for it to become actionable, Spencer says.
Claims data on any one patient is also plagued by incurred but not reported claims. Until IBNR claims get processed through Medicare or other payers, a true picture of a patient’s treatment is incomplete.
In light of this, it’s important for all concerned to have realistic expectations of what population health analytics can achieve and when, Spencer says.
“Cost is a practical concern we all face in our day-to-day lives,” he says. “You get more for more money, but as in all things, you have to be prudent. I don’t know how you will be able to do business in the very near future without using some form of analytics. How will your quality measures be good enough to meet the ‘gates’ required for contracts? How will you know where you are or if you can grow and how? It has cost a lot of money—money that’s been spent over a long period of time. The cost is into the low millions.
“That said,” Spencer adds, “we are able to take advantage of newer payment models that reward us not just for healthcare, but outcomes. We can potentially get paid for not doing anything—the PMPM that can be negotiated when you show you are doing a good job managing a population of patients.”
Analytics in the ambulatory practice
Gastroenterologist Tom M. Deas Jr., MD, practices as part of North Texas Specialty Physicians based in Fort Worth, an independent physician association comprising nearly 600 family and specialty doctors. NTSP has its own health plan and has been managing Medicare patients at risk for several years.
NTSP provided initial funding for a population health analytics firm, Sandlot Solutions, which has now been spun out as a separate company, although NTSP remains a part owner and Deas also serves as Sandlot’s chief medical officer. NTSP uses Sandlot’s analytics software to manage 80,000 at-risk lives, Deas says.
“Without some of the information technology to identify those patients based on their illnesses, comorbid illnesses, their severity of illness, who their physicians are, where they’ve been going to get their care, and being able to manage the whole spectrum of the care, you’re at a serious disadvantage,” Deas says.
Sandlot’s technology combines claims and clinical data into a robust patient data warehouse that helps meet some of the quality measures required to be an ACO, says Deas. “With the ACO, no matter how much money you save, you don’t get a dime of it if you haven’t met all the quality measures, so if we fall short in that area, it’s economically not good and it’s not good for the patients.”
By default, all Pioneer ACOs received three years of Medicare claims data. Getting the data into the warehouse requires overcoming some well-known healthcare IT issues, such as reconciling that claims data with an enterprise master-patient index, eliminating duplicates, and general patient-matching issues, Deas notes.
Once that was done, NTSP could concentrate on using Sandlot’s analytics to spot and eliminate wasteful services, as such home visits for patients lacking a medical necessity for such visits, Deas says. Analytics-driven interventions can manage a few hundred overutilizers of services as outpatients, focusing care management on them, he adds.
After a year’s effort, NTSP has bent its cost curve through these efforts to the tune of $50 per member per month, Deas says. “Now we’re not completely there,” he cautions. “It’s an incremental process, because you’re not only doing management, but you’re changing behaviors also. You’re trying to get patients aligned with the primary care physician, trying to move them from one source of care that was maybe excessive utilization to another.”
Deas says measuring the ROI of analytics technology remains elusive.
“A lot of people think they just buy an analytics tool and a data warehouse and an HIE and it’ll sit there and solve their problems,” he says. “That is not the case. You have to have human folks using that tool to manage the care of patients, to lower the cost and improve the quality. It’s like me asking you how much more efficient are you with a smartphone than you were five years ago with whatever version of phone you had then. You can’t answer that question. All you know, it’s just one part of what’s happened in the past five years to make you more efficient.”
It no doubt helps that NTSP’s executive director, Karen van Wagner, has a PhD in statistics, giving the organization added expertise to quantify results as they emerge.
Analytics technology is just beginning to make its impact felt in population health management. Careful consideration of products, objectives, workflows, and business conditions will steer providers through potential pitfalls, but the effort is considerable and the challenge to healthcare leadership is ongoing.
“Among the things that made these changes successful is an IT infrastructure that supports population health management and care management,” Deas says. “We still have to throw a fair amount of resources—human resources—at it to make it work.”
Reprint HLR1113-2
This article appears in the November issue of HealthLeaders magazine.
Scott Mace is senior technology editor at HealthLeaders Media.
 Farzad Mostashari, MD, stepped down from his post as the National Coordinator for Health Information Technology at the U.S. Department of Health and Human Services (HHS), during the first week of October, which was also the first week of the Federal partial shutdown. During his tenure, Dr. Mostashari, who
Farzad Mostashari, MD, stepped down from his post as the National Coordinator for Health Information Technology at the U.S. Department of Health and Human Services (HHS), during the first week of October, which was also the first week of the Federal partial shutdown. During his tenure, Dr. Mostashari, who  Paul Tarini, team leader for the
Paul Tarini, team leader for the  Daily text messaging may be a useful self-monitoring tool for weight control, particularly among racial/ethnic minority populations most in need of intervention, according to Duke University study results published in a Journal of Medical Internet Research
Daily text messaging may be a useful self-monitoring tool for weight control, particularly among racial/ethnic minority populations most in need of intervention, according to Duke University study results published in a Journal of Medical Internet Research