- The Affordable Care Act now lets employers charge employees different health insurance rates, based on whether they exercise, eat healthful foods and other “wellness” choices they make outside of work.
- As different phases of the law have taken effect and companies have better understood how to implement it, there basically have been three levels of wellness engagement:
- Level 1 encourages employees to join a wellness program with exercise and nutrition activities and undergo biometric screenings that check weight, body mass, cholesterol and other health indicators.
Level 2 trades the carrot for the stick. Employees (and insured family members) who don’t submit to the screening and participate in wellness programs face steep penalties; they may have to pay up to 30 per cent more for their share of health insurance costs.
- Level 3 in the march towards wellness adopts “outcomes” based programs that can require employees to meet specific fitness goals or pay higher insurance costs.
- WELLOGRAPH.com looks like an interesting prospect at AUD354
http://www.afr.com/p/technology/wearable_tech_privacy_headed_on_1uDsKFvA5cacLwe6vTKIBN
Wearable tech, privacy on collision course
PUBLISHED: 8 HOURS 48 MINUTES AGO | UPDATE: 4 HOURS 28 MINUTES AGO
 The Zepp Labs wearable sensor on a golf glove … this year’s Consumer Electronics Show was dominated by the next generation of fitness devices. With more advanced sensors and improved hardware.
The Zepp Labs wearable sensor on a golf glove … this year’s Consumer Electronics Show was dominated by the next generation of fitness devices. With more advanced sensors and improved hardware.
BRIER DUDLEY
Outrage over NSA spying is nothing compared to how people may react to the upcoming collision with wearable computing, medical privacy and new insurance rules.
You don’t need leaked documents to see it coming, though it took me a while to connect the dots after seeing the bewildering array of new health and fitness-tracking gadgets shown at January’s Consumer Electronics Show.
The show was seen as a turning point for “wearables”, including watches, wristbands, headsets and other gadgets. The most popular wearables monitor physical activity and connect wirelessly to phones, which may then upload the data to online services.
Research firms expect the fitness-wearables category to soar over the next few years, outpacing the growth of smartphones and tablets.
Not everyone wants to have a little computer on the wrist or head keeping track of what a wearer does around the clock. But I wonder if they won’t have much choice in the future, under new insurance laws in the US that invite companies to scrutinise and monitor their employees’ health and fitness.
In the past, medical information was generally none of your employer’s business. It’s still technically private. But the health-care overhaul known as Obamacare is chipping away at this wall.
The Affordable Care Act now lets employers charge employees different health insurance rates, based on whether they exercise, eat healthful foods and other “wellness” choices they make outside of work.
A 2013 survey by Aon Hewitt consulting found that motivating employees to change health behaviours is a “significant focus” over the next three to five years at 69 per cent of employers.
It doesn’t seem like a bad thing because it’s wrapped up in warm and fuzzy doublespeak. This isn’t about saving companies money; it’s about your health. Companies aren’t forcing you to participate, they’re offering rewards. We all want to be healthy, right?
As different phases of the law have taken effect and companies have better understood how to implement it, there basically have been three levels of wellness engagement.
TRACKING HEALTH
The first encourages employees to join a wellness program with exercise and nutrition activities and undergo biometric screenings that check weight, body mass, cholesterol and other health indicators.
Level 2 trades the carrot for the stick. Employees (and insured family members) who don’t submit to the screening and participate in wellness programs face steep penalties; they may have to pay up to 30 per cent more for their share of health insurance costs.
The law calls this a “reward” for participation. Flip it around and it’s a penalty for not authorising your employer to manage and monitor how you live outside of work.
Better health overall is in everyone’s best interest. But you can’t help but be cynical when it becomes tied to benefit levels, especially in an era of vanishing pensions, flat pay cheques and longer work days.
It’s too early to say whether wellness programs will make a big difference. In the meantime, they can change the workplace dynamic.
By insinuating that individual choices are the driver of health-care costs, they erode the social contract of group plans in which everyone contributes to coverage that takes care of each other and their families in case something happens.
I’m digressing.
Level 3 in the march towards wellness adopts “outcomes” based programs that can require employees to meet specific fitness goals or pay higher insurance costs.
At this point, when body tracking and measurements are used to adjust benefits, it gets harder to maintain the pretence of privacy. Even if individual records are masked, the data will provide enough insight to assess employees’ potential health costs as well as job performance, enabling a new form of discrimination.
Aon Hewitt’s survey said 64 per cent of employers that offer health-care coverage are using data to find cost savings and as they shift towards health-improvement strategies, they’re relying “more on integrated, dynamic data aggregation tools to laser in on the best opportunities for reduction of unnecessary costs”.
TECHNOLOGY ADVANCEMENTS HELP MONITORING
Tech companies are ahead of the game. One is Limeade, a hot start-up in Bellevue that last year doubled sales of its software platform, which employers and insurance companies use to encourage and monitor wellness activities. The platform can sync with dozens of fitness-tracking devices and apps.
Last month’s Consumer Electronics Show was dominated by the next generation of fitness devices. With more advanced sensors and improved hardware, they’re building on the success of activity trackers such as the Fitbit and Nike FuelBand that millions of people — including me — already use. Show organisers gave an “innovation award” to the $US320 ($354) Wellograph Watch, which includes a continuous heart-rate monitor, wellness tracker and running watch in a sleek case.
Fitness tracking may become hard to avoid. Intel unveiled sensors at CES that can be embedded into common devices such as earbuds, which then track physical activity. The data can be relayed to a wellness app on a phone and online wellness programs.
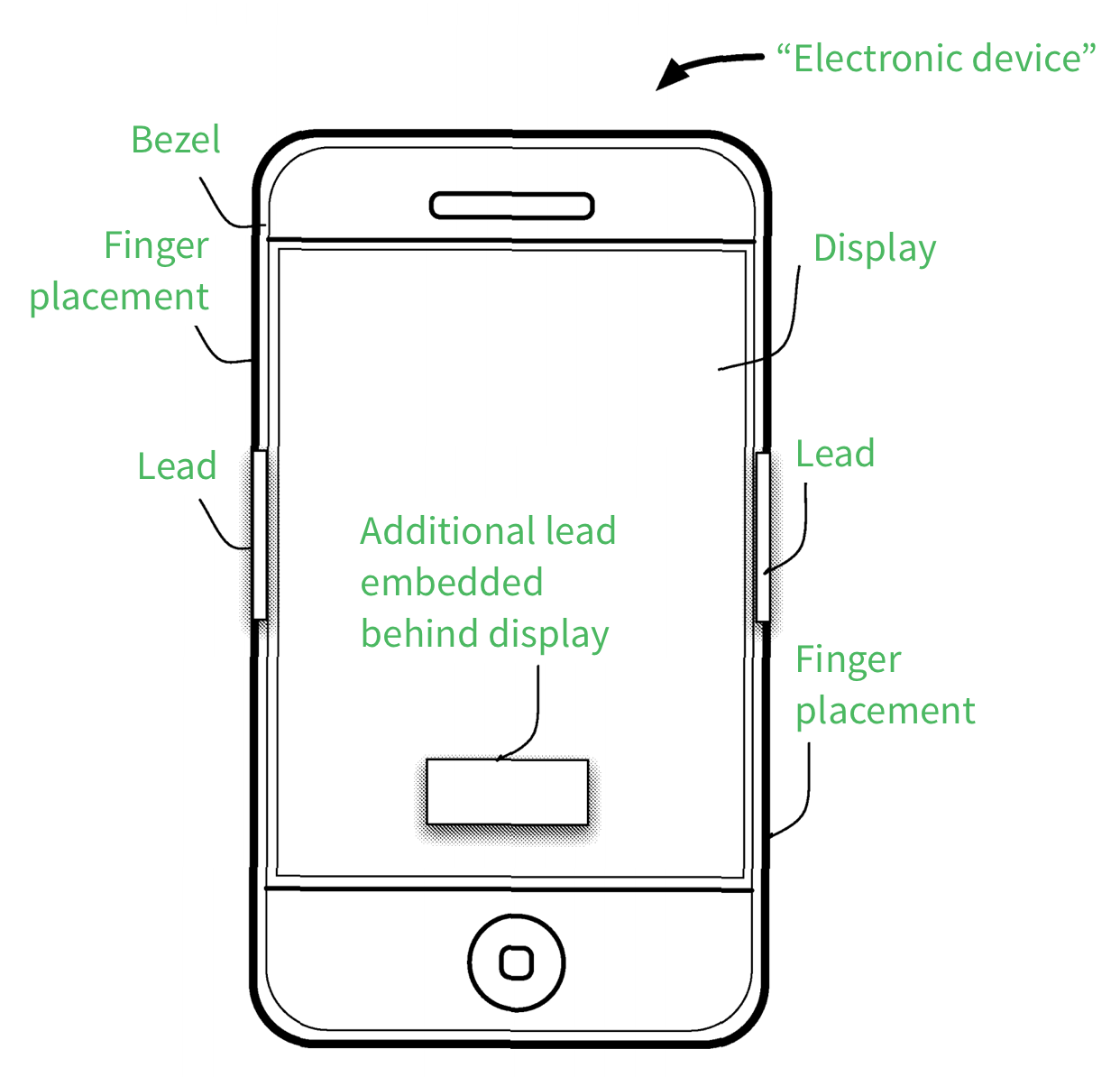
Apple also is chasing this opportunity. With the iPhone 5S, it began using a processor with built-in sensors that can be used by fitness apps.
On January 31, word surfaced that Apple had a big meeting with the Food and Drug Administration, apparently to discuss medical apps and perhaps its own version of a health-monitoring watch. This isn’t too surprising. After years of back and forth with tech companies and others, the FDA in September issued guidelines for health-related apps and gadgets, to clarify which will be considered medical devices and require regulatory approval.
I suggest regulators go a step further and issue privacy guidelines for wellness programs, health apps and wearable devices that may share data with insurers and employers. They could be modelled on the Miranda warnings that police use, informing people of their right to avoid self-incrimination under the Fifth Amendment:
“You have the right to keep your health information private, anything you disclose about your health can and will be used against you.”