All posts by blackfriar
What can be more immoral than the vicarious redemption of sin?
What can be more immoral than the vicarious redemption of sin?
Lindsay Scheske 37 mins ago Easter Sunday, 2014
Facebook Post
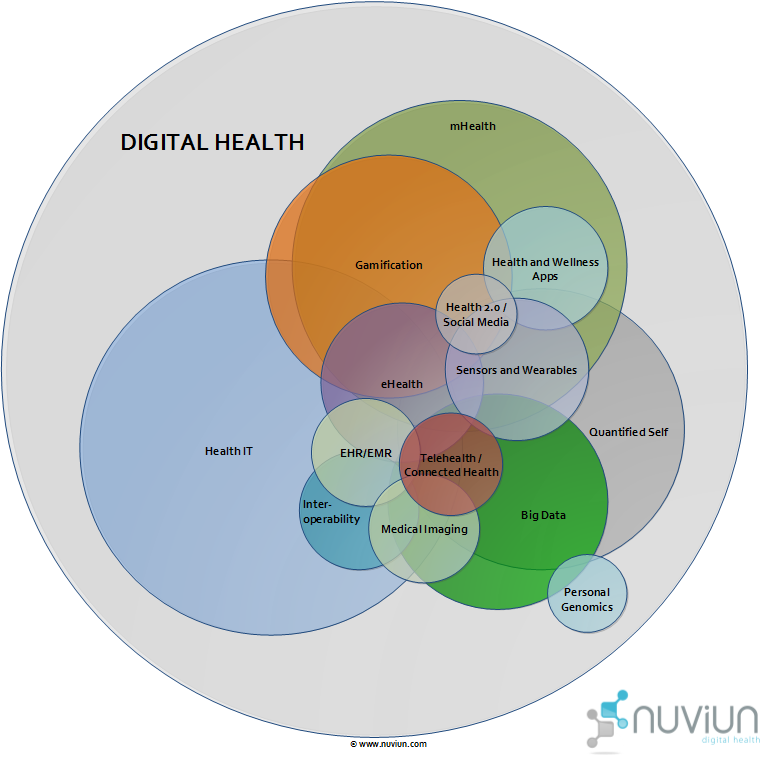
The Story of Digital Health
http://www.nuviun.com/nuviun-digital-health
good infographics…
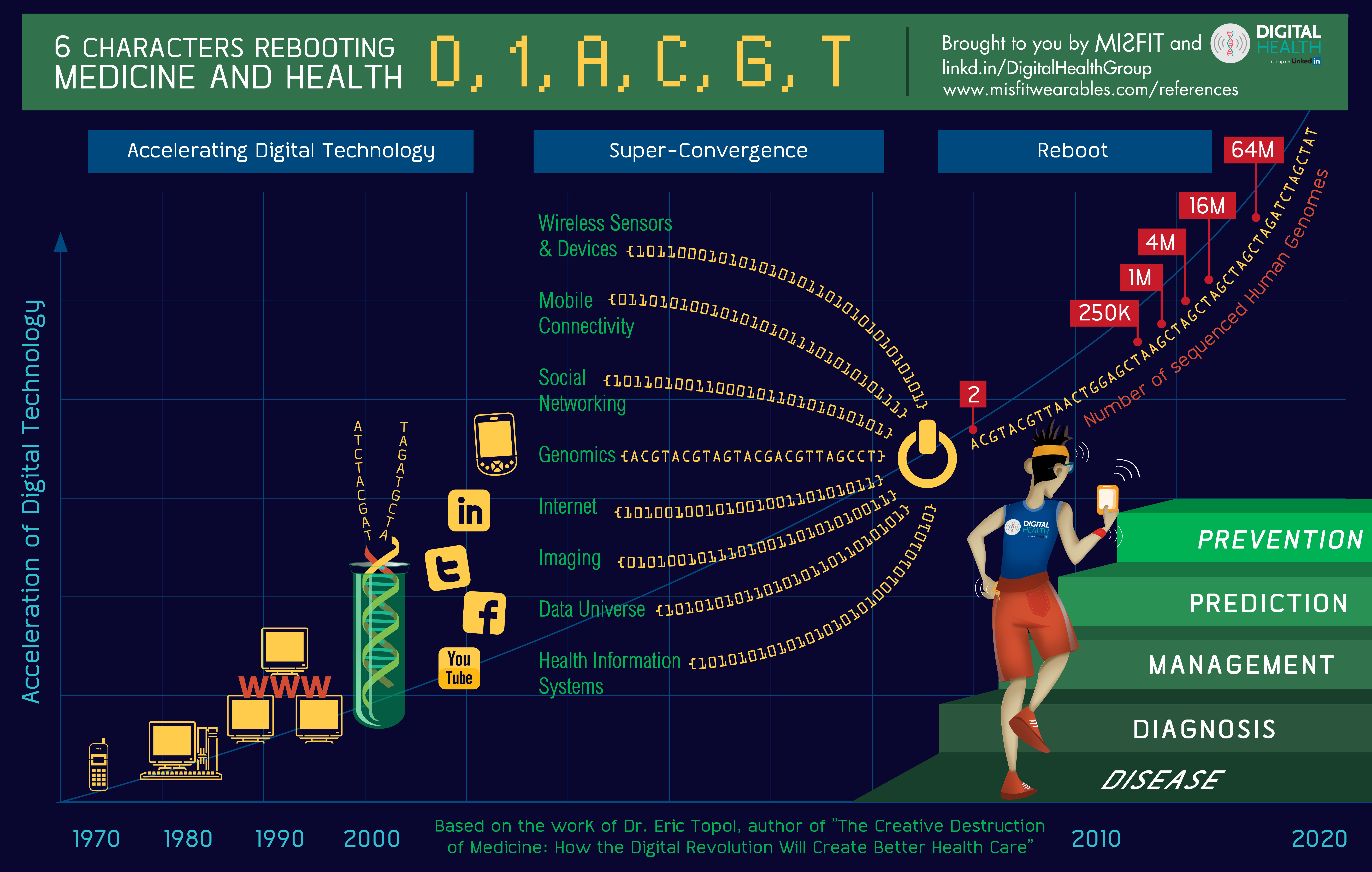
http://storyofdigitalhealth.com/infographic/
Infographic
I created this conceptual infographic illustrating the increasing health benefits achievable with digital health with the great team at Misfit Wearables. You can download a high-resolution version by clicking on the image.
References:
Number of people sequenced
“250,000 human genomes will be fully sequenced by the end of 2012, 1 million by 2013, and 5 million by 2014″ -Topol, Eric (2011-12-02). The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care (p. 102). Perseus Books Group. Kindle Edition.
Also, compliments of Story of Digital Health strategic partner nuviun, there’s this interactive diagram of the digital health landscape…
PCMH & ACO complementarity requires policy evolution
PCMHs and ACOs are complementary approaches to improving care delivery. Medical homes require strong links to specialists and hospitals, while ACOs—which are accountable for the full continuum of health services—require a strong grounding in primary care. The authors suggest the following payment approaches to promote integration of PCMHs and ACOs:
- ACO contracts could include dedicated payments to support enhanced primary care services.
- ACOs could invest in PCMHs by hiring more primary care providers, expanding office hours, developing information technology and care coordination infrastructure, supporting coaching and learning collaboratives, and dedicating resources to urgent care.
- ACOs could align physician performance and resource allocation to support PCMHs. For example, measures of care coordination and communication could be considered when assessing physician performance. Primary care physicians could be paid according to the size and complexity of their patient panels, and specialists could be given incentives to work with medical homes.
http://www.commonwealthfund.org/Publications/In-Brief/2014/Apr/Structuring-Payment-to-Medical-Homes.aspx?omnicid=20
Structuring Payment to Medical Homes After the Affordable Care Act
April 7, 2014
Authors: Samuel T. Edwards, Melinda K. Abrams, Richard J. Baron, Robert A. Berenson, Eugene C. Rich, Gary E. Rosenthal, Meredith B. Rosenthal, and Bruce E. Landon
Journal: Journal of General Internal Medicine, published online April 1, 2014
Contact: Bruce E. Landon, M.D., M.B.A., Harvard Medical School, landon@hcp.med.harvard.edu
Summary Writers: Martha Hostetter
Access to full article: View Article
The Issue
The patient-centered medical home (PCMH) model aims to transform primary care practice through the use of multidisciplinary teams and a shift from “reactive visit-based care to proactive population health management.” Currently, medical home providers are reimbursed with a blend of fee-for-service payments and additional compensation for services provided outside of office visits, including care coordination. Writing in the Journal of General Internal Medicine, Harvard Medical School’s Samuel T. Edwards, M.D., and colleagues consider how the PCMH payment model could evolve to keep pace with health care payment reforms launched by the Affordable Care Act, most notably the “shared savings” approach used by many accountable care organizations (ACOs).
What the Study Found
PCMHs and ACOs are complementary approaches to improving care delivery. Medical homes require strong links to specialists and hospitals, while ACOs—which are accountable for the full continuum of health services—require a strong grounding in primary care. The authors suggest the following payment approaches to promote integration of PCMHs and ACOs:
- ACO contracts could include dedicated payments to support enhanced primary care services.
- ACOs could invest in PCMHs by hiring more primary care providers, expanding office hours, developing information technology and care coordination infrastructure, supporting coaching and learning collaboratives, and dedicating resources to urgent care.
- ACOs could align physician performance and resource allocation to support PCMHs. For example, measures of care coordination and communication could be considered when assessing physician performance. Primary care physicians could be paid according to the size and complexity of their patient panels, and specialists could be given incentives to work with medical homes.
Conclusions
As a promising model of care delivery, the PCMH “can serve as a lynchpin of ACOs,” the authors say. For their part, ACOs will need to support this model within their organizations.
Citation
S. T. Edwards, M. K. Abrams, R. J. Baron et al., “Structuring Payment to Medical Homes After the Affordable Care Act,” Journal of General Internal Medicine, published online April 1, 2014.
Community factors (SDH?) drive readmissions
- 60% of variation in readmissions is driven by location, not care!
- More GPs > fewer readmissions.
- More specialists > more readmissions.
PDF: 1742_Herrin_community_factors_hosp_readmission_rates_HSR_04_09_2014_itl
Community Factors and Hospital Readmission Rates
April 16, 2014
Authors: Jeph Herrin, Justin St. Andre, Kevin Kenward, Maulik S. Joshi, Anne-Marie J. Audet, and Stephen C. Hines
Journal: Health Services Research, published online April 9, 2014
Contact: Jeph Herrin, Ph.D., Division of Cardiology, Yale University School of Medicine, jeph.herrin@yale.edu
Summary Writers: Deborah Lorber
Access to full article: View Article
“The current readmission reduction program that aims to penalize hospitals whose readmissions are above a certain threshold may not be appropriate.”
Synopsis
A majority of the variation seen in U.S. hospitals’ readmission rates for heart attack, heart failure, and pneumonia can be attributed to hospitals’ location, rather than to the quality of care provided in individual hospitals. Community factors most strongly associated with lower hospital readmission rates include more general practitioners and fewer specialists per capita and the presence of high-quality nursing home care.
The Issue
Readmission to the hospital shortly after discharge has been recognized as an indicator of poor health system coordination. Since 2009, the Centers for Medicare and Medicaid Services has been publicly reporting 30-day readmission rates for heart attack, heart failure, and pneumonia. And in 2013, Medicare began linking payments to hospitals to how well they perform on these measures, leading hospitals to focus on improving their rates. Previous studies have looked for relationships between readmission rates and hospital characteristics, like size or teaching status, or patient-level factors, like race or health literacy. This article, supported by The Commonwealth Fund, looks at the association between readmission rates and local community characteristics.
Key Findings
- Almost 60 percent of the variation in U.S. hospital readmission rates can be explained by the county where a hospital is located. Individual hospital performance accounts for only two-fifths of the variation for the three conditions examined.
- Having high percentages of residents who are Medicare beneficiaries, are unemployed, or have never been married is associated with higher hospital readmission rates. However, an area’s designation as a “retirement destination” was associated with lower rates—a possible reflection of higher socioeconomic status among the Medicare population and a community geared toward caring for older people.
- Higher numbers of general practitioners per capita were associated with lower readmission rates, while higher numbers of specialists were associated with higher readmission rates.
- In counties where nursing home quality was higher (as measured by multiple indicators), readmissions were lower.
Addressing the Problem
If community factors explain a substantial amount of the variation in hospital readmission rates, then programs that penalize hospitals with readmission rates above a certain threshold may not be appropriate, the authors say. Other initiatives might be more effective, such as the Affordable Care Act’s Community-Based Care Transitions Program, which allows community-based organizations to receive a bundled payment that covers the costs of services needed to help patients transition from hospital to home.
About the Study
The authors examined all hospitals with publicly reported 30-day readmission rates for patients with acute myocardial infarction, heart failure, or pneumonia who were discharged between July 1, 2007, and June 30, 2010. Readmissions data were then linked with publicly available county data from the Area Resource File, the U.S. Census, Nursing Home Compare, and the Neilsen PopFacts data set. The final sample included 4,073 hospitals.
The Bottom Line
Population characteristics at the county level explain a large portion of the variation in hospital readmission rates for certain major medical conditions. Instead of strictly penalizing hospitals for exceeding certain thresholds, policymakers should focus on programs that help patients transition from hospital to home.
Citation
J. Herrin, J. St. Andre, K. Kenward et al., “Community Factors and Hospital Readmission Rates,” Health Services Research, published online April 9, 2014.
New medical data allows comparison shopping
“Whenever you put information out there, creativity and innovation flourish,” she said. “This is going to be such a giant leap forward in terms of what we’re doing in health care today, what works, what doesn’t work and what it should cost.” But for that to happen “there needs to be some “pretty powerful computing and some savvy tech gurus to help slice and dice this information in meaningful ways for consumers”
New York is sponsoring a contest — the Health Innovation Challenge — that asks the tech-savvy, including coders and developers, to put health data to use keeping costs down, increasing quality and improving efficiency. Winners receive cash, and their ideas will be put to work in the state government.
Shah said releasing the data — and allowing researchers, entrepreneurs and consumers to dig into it — could “democratize” health care in a way that has already happened with the way people buy cars or plane tickets: It will allow them to compare cost and quality.
Instead of making decisions based on quality, people tend to pick their providers based on where their doctor recommends they should go, and that might mean where she did her residency or a specialist whom she plays golf with, he said. New data may allow people to comparison shop for medical care.
While Shah acknowledged a “special” relationship between a patient and a doctor that includes treatment plans and communication in ways that won’t be picked up in data, a colonoscopy should be the same everywhere.
Rather than taking doctors’ recommendations, entrepreneurs will take data, repackage it and show people which hospitals have the longest average stays, which charge the most for a procedure, and which have the highest infection rates.
“Often, we find that high quality equals lower costs,” he said. That’s because the most cost-effective procedures tend to be the ones where patients receive proper medications, do not have to be treated for hospital-based infections, and where providers work as a team to make sure quality measures are met.
As more people — or their employers — choose low-premium, high-deductible plans, the cost of a knee surgery or an imaging scan becomes more important to the consumer than when insurance covered everything.
http://www.usatoday.com/story/news/nation/2014/04/16/new-cms-data-inspires-entrepreneurs/7735469/
WASHINGTON — As the government moves toward more medical “transparency” by releasing a slew of new data— including Medicare provider payment data last week — entrepreneurs are creating new products to help consumers use the data to choose quality, lower-cost care.
Beyond the profit motive, some entrepreneurs hope to use the data to keep costs down on new medical products they create, help the government suss out fraud or unusual activity, and to persuade doctors to use the best practices gathered from their peers — something that was difficult to do when pricing information was not available.
CHART: See how much Medicare paid each doctor in U.S.
“I think this data transparency is one of the major keys to transformation of the entire health care system,” said Robert Grajewski, president of Edison Nation Medical, a group that works to remove barriers for getting medical devices to the market. “In health care, it’s very confusing to know what the pricing is, not just for the device, but for the overall procedure. This helps us have a benchmark that needs to be achieved or overcome to improve care and overcome costs.”
The provider payment data released by the Centers for Medicare & Medicaid Services has Grajewski looking at why prices are higher for one doctor over another, why a doctor might choose a brand name over a generic medication, and why a doctor might choose surgery over physical therapy. The data became available after a court order lifted an injunction sought by the American Medical Association had been in place since 1979.
Grajewski isn’t the only one. Mercom Capital Group released a report Monday that found venture capital funding for health care information technology hit $858 million in the first quarter of this year. That includes $398 million in 103 new deals for consumer-focused technology, such as mobile apps.
“We’ve been tracking these numbers since 2010, and this quarter was the biggest number ever,” said Raj Prabhu, Mercom’s CEO. “$858 million is a huge number — in 2010, I don’t think we saw $200 million.”
Much of the momentum is coming from inventors who hope to create shopping applications that allow consumers to compare prices and outcomes on their smart devices. These include apps such as GoodRX, which allows consumers to compare medication prices at different pharmacies; NerdWallet Health, which allows people to compare hospital prices by locations; and an app from Consumer Reports that lets people compare prices for hip and knee replacements.
“Ever since the government started releasing data, this has been great for these kinds of companies to turn into useful applications,” Prabhu said.
“Every person is a health care consumer,” he said. “It’s so massive — nobody wants to miss the boat.”
Ceci Connolly, managing director of PWC’s Health Research Institute, said she expects the data to ultimately help the health care industry itself.
“Whenever you put information out there, creativity and innovation flourish,” she said. “This is going to be such a giant leap forward in terms of what we’re doing in health care today, what works, what doesn’t work and what it should cost.”
But for that to happen, there needs to be some “pretty powerful computing and some savvy tech gurus to help slice and dice this information in meaningful ways for consumers,” she said. Someone could use the CMS data to look at trends in hip surgeries: Is it much higher for one hospital than at others? A consumer might reconsider whether he actually needs surgery from a particular doctor. Or are there relatively few hip surgeries at the local hospital? The consumer might consider going to a doctor who performs a lot of hip surgeries.
Someone else might take the CMS data and compare it to CMS’s Five-Star Quality Rating System data, Connolly said.
“The whole promise of big data is not just any one data set, but it’s the way you can bring them together and analyze them across many,” she said.
New York is sponsoring a contest — the Health Innovation Challenge — that asks the tech-savvy, including coders and developers, to put health data to use keeping costs down, increasing quality and improving efficiency. Winners receive cash, and their ideas will be put to work in the state government.
It comes after the launch of the state’s transparency project, Open.NY.gov, which features data that state agencies have been ordered to catalog for the public.
“For a long time, the medical establishment has talked about patient-centered care,” New York State Department of Health Commissioner Nirav R. Shah. “But largely, it’s still been about hospital-centered care, doctor-centered care.”
Shah said releasing the data — and allowing researchers, entrepreneurs and consumers to dig into it — could “democratize” health care in a way that has already happened with the way people buy cars or plane tickets: It will allow them to compare cost and quality.
Instead of making decisions based on quality, people tend to pick their providers based on where their doctor recommends they should go, and that might mean where she did her residency or a specialist whom she plays golf with, he said. New data may allow people to comparison shop for medical care.
While Shah acknowledged a “special” relationship between a patient and a doctor that includes treatment plans and communication in ways that won’t be picked up in data, a colonoscopy should be the same everywhere.
Rather than taking doctors’ recommendations, entrepreneurs will take data, repackage it and show people which hospitals have the longest average stays, which charge the most for a procedure, and which have the highest infection rates.
“Often, we find that high quality equals lower costs,” he said. That’s because the most cost-effective procedures tend to be the ones where patients receive proper medications, do not have to be treated for hospital-based infections, and where providers work as a team to make sure quality measures are met.
As more people — or their employers — choose low-premium, high-deductible plans, the cost of a knee surgery or an imaging scan becomes more important to the consumer than when insurance covered everything.
PCORI: US begins significant data linking foray to investigate comparative effectiveness
- Patient Centered Outcomes Research Institute (PCORI) NIH-funded 10 site data linking project hoping to develop a complete clinical picture of 26-30 million Americans
- Do certain sets of behavioral interventions work better than others for weight control? Might certain antibiotics work better for cystic fibrosis patients, based on their genetic profile?
- It’s described in the story as the holy grail of health-care research, but it doesn’t incorporate social determinants, so how can it be? (PN)
http://www.washingtonpost.com/national/health-science/scientists-embark-on-unprecedented-effort-to-connect-millions-of-patient-medical-records/2014/04/15/ea7c966a-b12e-11e3-9627-c65021d6d572_story.html
Scientists embark on unprecedented effort to connect millions of patient medical records
The data — from every patient treated at one of New York’s major hospital centers over the past few years — include some of the most intimate details of a life. Vital signs. Diagnoses and conditions. Results of blood tests, X-rays, MRI scans. Surgeries. Insurance claims. And in some cases, links to genetic samples.
Nothing of this scale has been built before, and researchers say the potential of the network to speed up research efforts and to answer questions that have long vexed scientists cannot be overstated. But the creation of the network presents tricky ethical questions about who owns and controls the data, how to protect patient privacy and how research questions will be prioritized.
“Both the opportunity and the anxiety are pretty electrifying,” Francis S. Collins, director of the National Institutes of Health, said in an interview.
The origins of the patient project lie in an obscure part of the 2010 Affordable Care Act. As part of the nation’s health-care overhaul, Congress created an independent nonprofit group to help patients and their doctors make better-informed decisions about care. Dubbed the Patient-Centered Outcomes Research Institute, or PCORI, and based in the District, the organization’s mandate is to launch, fund and coordinate research on “comparative effectiveness” — to find out which drugs, devices and treatment options are more effective than others.
Do certain sets of behavioral interventions work better than others for weight control, for example? Might certain antibiotics work better for cystic fibrosis patients, based on their genetic profile?
Such questions have been surprisingly difficult to answer, despite the thousands of clinical trials published every year.
Physicians have long grumbled that few studies can be translated into practical advice. Some studies are too small to draw any definitive conclusions. Others include patients diagnosed with a single condition, while most patients are more complicated — they suffer from multiple issues. It isn’t uncommon for studies to contradict each other, and there’s no way for clinicians to know which one is right, because they often use different methodologies.
“The whole idea was to create a way to do the kind of research that would inform the real world,” explained Eugene Rich, who researches health-care effectiveness for Mathematica Policy Research, based in Princeton, N.J.
The database — an idea that has been talked about for years by everyone from insurance companies to Google but has never been successfully executed — holds the hope that some of those obstacles can be overcome.
“We will be able to get answers with a degree of certainty that we’ve never had before,” said Joe V. Selby, PCORI’s executive director, who calls the patient records network “the holy grail” of health-care research.
Collins said the value of the network is that it gives scientists the ability to ask an endless number of questions about a massive patient population with great speed and little cost.
In the randomized trials that NIH typically supports, “you have to enroll patients from the very beginning, and that’s a big infrastructure-building process that can take quite some time. And once a trial has been conducted, the whole thing has to be taken down again,” Collins said.
“It’s a great way to answer one specific question, but it’s not an efficient way to ask lots of questions,” he explained.
Before PCORI’s vision can be realized, the project’s leaders must overcome numerous hurdles.
The technical challenges of the project are enormous. The specter of the botched launch of HealthCare.gov haunts anyone trying to get large numbers of separate computer systems to talk to each other. But it is the larger questions about governance that have triggered conflict and worry in the nation’s health-care community.
How will research questions be prioritized? How should disagreements be resolved?
Should pharmaceutical companies and insurers be able to access the records and, if so, under what circumstances? What about the Centers for Disease Control and Prevention? The information could help epidemiologists track outbreaks and clusters of disease in a way they have never done before.
And, critically important to the multibillion-dollar pharmaceutical industry, how will the Food and Drug Administration view this type of research when considering applications for new drugs or in recalling old ones?
PCORI was never imagined to be the custodian of this kind of data network. It was designed to launch and fund research in a manner similar to NIH and the National Science Foundation. But it did not get nearly the same kind of funding.
President Obama’s budget request for fiscal 2015 included $30.4 billion for NIH and nearly $7.3 billion for NSF. But PCORI, which is funded through several streams, gets only about $500 million annually. Large, randomized clinical trials such as the ones NIH does for important questions cost upwards of $150 million, meaning that PCORI has enough to fund only two or three a year.
“So about a year ago, PCORI started talking about whether there is another model that is different from the NIH model, which would be more about embedding clinical studies in the fabric of day-to-day care,” said Robert W. Dubois, chief science officer for the National Pharmaceutical Council, a health policy research group funded by the industry.
The PCORI network, which is being built at a cost of nearly $100 million, would also be a way to pinpoint patients with certain criteria who could be invited to join a clinical trial. As it stands today, identifying patients eligible for trials is often time-consuming, expensive and hit-or-miss. Researchers must use a variety of tools to get enough participants, including reaching out to a network of doctors who then contact their patients and the old-fashioned method of putting up fliers in places where people with the criteria they are looking for congregate.
The new national patient network will comprise 11 sub-networks that include records from New York and Chicago, children’s hospitals, Kaiser Permanente and other groups. Each participating organization retains all the personally identifiable data and would have the right to accept or decline a research proposal. If a research project is greenlighted, each of the smaller networks would analyze its own databases and return an anonymized, aggregated response to the researcher.
“The raw data is not what is being shared. That remains with the institution that the patient trusts,” said Devon McGraw, director of the health privacy project for the Center for Democracy and Technology and head of the data privacy task force for PCORI.
Privacy experts say the general consent forms that patients sign when they get treatment should allow the use of data already collected in the aggregate. Hospitals and other organizations participating in the project don’t have any plans to explicitly inform patients about this. If researchers wanted doctors to collect additional data as part of a clinical trial, the researchers would clearly have to get a patient’s consent. But what about projects that involve more detailed analysis of individual patient histories?
One aspect of the project that was highlighted by researchers involved is that it has included patients at every step. Patient panels have been convened to help suggest research questions, and patients serve on the committees looking at privacy and data security.
“As a provider, I may be interested in how a serum marker changes with a treatment. But patients may be more interested in how it affects how they feel, their ability to exercise and eat,” she said.
Brian Currie, vice president for medical research for the Montefiore Medical Center, the university hospital for the Albert Einstein College of Medicine in the Bronx, which is participating in the New York network, said the number of questions are understandable given the historical barriers between different types of institutions that have prevented this research in the past.
“It’s pushing all the fronts on how medical institutions do research,” Currie said.
US Healthcare Price Transparency
An interesting observation – unintended consequence of non-universal healthcare?: As consumers are being asked to pay more, so they’re trying to become better health-care shoppers.
- states have passed transparency laws
- medicare has started to dump raw service cost data
- private firms are developing their own transparency tools
- a report recommends:
- total estimated price
- out-of-pocket costs
- patient safety and clinical outcome data
“Care providers, employers and health plans have negotiated rates, which isn’t necessarily something they want out in the public. They warn making those negotiations publicly could actually discourage negotiations for lower prices — naturally, there are conflicting opinions on this point.”
http://www.washingtonpost.com/blogs/wonkblog/wp/2014/04/16/price-transparency-stinks-in-health-care-heres-how-the-industry-wants-to-change-that/

Price transparency stinks in health care. Here’s how the industry wants to change that.
By Jason Millman
There’s been much written in the past year about just how hard it is to get a simple price for a basic health-care procedure. The industry has heard the rumblings, and now it’s responding.
About two dozen industry stakeholders, including main lobbying groups for hospitals and health insurers, this morning are issuing new recommendations for how they can provide the cost of health-care services to patients.
The focus on health-care price transparency — discussed in Steven Brill’s 26,000-word opus on medical bills for Time last year — has intensified, not surprisingly, as people are picking up more of the tab for their health care. Employers are shifting more costs onto their workers, and many new health plans under Obamacare feature high out-of-pocket costs.
The health care-industry has some serious catching up to do on the transparency front. States have passed their own health price transparency laws, Medicare has started to dump raw data on the cost of services and what doctors get paid, and private firms have developed their own transparency tools.
“We need to own this as an industry. We need to step up,” said Joseph Fifer, president and CEO of the Healthcare Financial Management Association, who coordinated the group issuing the report this morning. The stakeholder group includes hospitals, consumer advocates, doctors and health systems.
Their recommendations delineate who in the health-care system should be responsible for providing pricing information and what kind of information to provide depending on a person’s insurance status. Just getting the different stakeholders on the same page was difficult enough in the past, said Rich Umbdenstock, president and CEO of the American Hospital Association.
“We couldn’t agree on whose role was what. We were using terms differently,” he said.
The report’s major recommendations include how to provide patients with:
- the total estimated price of the service
- a clear indication of whether the provider is in-network or where to find an in-network provider
- a patient’s out-of-pocket costs
- and other relevant information, like patient safety scores and clinical outcomes.
“I think that the focus now, unlike three years ago when it was on access, the focus is about affordability,” said Karen Ignagni, president and CEO of America’s Health Insurance Plans. “What are the prices being charged? It leads consumers to want to know, ‘How do I evaluate all that?'”
To give a sense of just how murky health pricing can be, one of the group’s recommendations is for providers to offer uninsured patients their estimated cost for a standard procedure and to make clear how complications could increase the price. You would think that shouldn’t be too hard — there’s no insurer to deal with, no contracts to consult.
But previous research points out just how difficult it can be to get the price for a basic, uncomplicated procedure. In a study published this past December, researchers found that just three out of 20 hospitals could say how much an uninsured person should expect to pay for a simple test measuring heartbeat rate.
The group’s recommendations also touches on limits to transparency and the “unintended consequences” of too much data being public. Care providers, employers and health plans have negotiated rates, which isn’t necessarily something they want out in the public. They warn making those negotiations publicly could actually discourage negotiations for lower prices — naturally, there are conflicting opinions on this point.
The report nods to other ways at achieving transparency. For example, it talks about “reference pricing” in self-funded employer health plans, in which employers limit what they’ll pay for an employee’s health-care services — thus setting the reference price.
“The employer communicates to employees a list of the providers who have agreed to accept the reference price (or less) for their services. If an employee chooses a provider who has not accepted the reference price, the employee is responsible for the amount the provider charges above the reference price,” the report reads, noting that Safeway grocery stores implemented a successful pilot program that expanded a few years ago.
Perhaps what’s most significant about these recommendations is the stakeholders’ acknowledgement that the health-care market is changing. Consumers are being asked to pay more, so they’re trying to become better health-care shoppers
AHIP’s Ignagni said most insurers already provide cost calculator tools and quality data on their Web sites. Providers, said the AHA’s Umbdenstock, need to be more accommodating to patients’ price-sensitivity.
“‘We can’t answer your question’ may have worked in the past, but it doesn’t fly any longer,” said Mark Rukavina, principal with Community Health Advisors and a report contributor. “This [report] basically lays out the principles for creating a new response to the question.”
Jason Millman covers all things health policy, with a focus on Obamacare implementation. He previously covered health policy for Politico. He is an unapologetic fan of the New York Yankees and Giants, though the Nationals and Teddy Roosevelt hold a small place in his heart. He’s on Twitter.
Guacamole
- 2 ripe avocados, halved, stones removed, peeled
- 1 small red onion, finely chopped
- 1 ripe tomato, finely chopped
- 2 garlic cloves, crushed
- 1 small fresh red chilli, deseeded, finely chopped
- 60mls (1/4 cup) fresh lime juice
- Salt & ground black pepper, to taste
- Step 1
Place the avocado flesh in a medium bowl and use a fork to mash until almost smooth.
- Step 2
Add the onion, tomato, garlic, chilli and lime juice and use a spoon to mix well. Taste and season with salt and pepper.
Note: This guacamole will keep for up to 1 day in an airtight container in the fridge. Serving suggestions: spread on sliced Italian bread instead of butter and top with sliced ripe tomatoes, torn rocket leaves, salt and pepper; or serve with homemade pits chips.
From: http://www.taste.com.au/recipes/10934/guacamole
GE’s Talent-Review System
http://blogs.hbr.org/2014/04/the-secret-ingredient-in-ges-talent-review-system/
Interesting (extremely high level) observations on the importance of dedicating time to people/performance issues.
The Secret Ingredient in GE’s Talent-Review System
As the custodian of the talent-review process, I have been lucky to observe this at close quarters. Here is what I’ve learned.
It starts with the attention given to the individual appraisal. Managers are expected to dedicate time to prepare for a detailed discussion of a direct report’s performance and values, strengths, development needs, and development plans. Most employees spend over 1,800 hours a year working for the manager and the company. Is it unreasonable to expect the manager to spend at least a few hours thinking about and discussing the performance appraisal as part of a larger commitment to helping the employee be more successful? (More about that in a moment.) Individual appraisals are considered enormous opportunities for the candid, constructive conversations that employees deserve.
It is not uncommon for a manager’s assessment and feedback to be questioned by his or her own manager, if the commentary does not appear to reflect the individual accurately. I have seen our top leaders return an appraisal because it did not do justice to the feedback on the individual. Such a disconnect is the worst thing that can happen because it is a reflection of the manager, or the HR manager, as much as it is of the employee. This practice of multi-level engagement ensures that the quality of the appraisal is honest and comprehensive.
We continue to use a nine-block grid with quadrants that capture levels of performance and values not as a means of a forced ranking but as a way of facilitating differentiation.Here is how it is done. As our businesses and functions go through the process, the leaders justify the positioning of talent in different quadrants of the grid. The system allows us to link the grid straight to the appraisal. The chairman sets the overall tone and expectations, and leaders across the company make suggestions, comments, and additions to the feedback. While each leader may only have visibility into his or her particular business, the system ensures consistency and provides a consistent view and assessment of talent across the company.
Most of our leaders, including the chairman, spend at least 30% of their time on people-related issues. It’s part of our operating rhythm. These discussions are rich in making calls on leadership, succession, opportunities for development, organization and talent strategy, diversity, and global talent builds. The discussions also afford us the opportunity to assess performance more closely and holistically − including market factors, internal factors, organizational complexity, and risk elements. More importantly, it is the business leaders who take the lead on these discussions, not the HR person. This is consistent with our philosophy that talent development and assessment is a key business agenda, not just an HR activity.
Some skills are more important than others to be a great leader. As I have observed these discussions, some of the patterns are becoming increasingly obvious to me. For instance, the difference between a great leader and a good one is not just about intellectual capacity; it is often about judgment and decision-making. Likewise, a hunger to win, tenacity, customer advocacy, and resourcefulness can trump some of the skills we often look for − analytical skills, for instance. Such traits are best unearthed through discussions and become important considerations for future talent mapping.
Effective talent review is an intensely human process that calls for extensive demands on a leadership’s time. There are no formulas or equations. The power lies in giving people the attention, candid feedback and mentoring they deserve through a company-wide commitment to human-capital development.