 Farzad Mostashari, MD, stepped down from his post as the National Coordinator for Health Information Technology at the U.S. Department of Health and Human Services (HHS), during the first week of October, which was also the first week of the Federal partial shutdown. During his tenure, Dr. Mostashari, who spoke at TEDMED 2011 with Aneesh Chopra, led the creation and definition of meaningful use incentives and tenaciously challenged health care leaders and patients to leverage data in ways to encourage partnerships with patients within the clinical health care team.
Farzad Mostashari, MD, stepped down from his post as the National Coordinator for Health Information Technology at the U.S. Department of Health and Human Services (HHS), during the first week of October, which was also the first week of the Federal partial shutdown. During his tenure, Dr. Mostashari, who spoke at TEDMED 2011 with Aneesh Chopra, led the creation and definition of meaningful use incentives and tenaciously challenged health care leaders and patients to leverage data in ways to encourage partnerships with patients within the clinical health care team.
Whitney Zatzkin and Stacy Lu had the opportunity to speak with Dr. Mostashari during his last week in office.
WZ: Sometimes, a person will experience an “aha!” moment – a snapshot or event that reveals a new opportunity and challenges him/her to pursue something nontraditional. Was there a critical turning point when you figured out, ‘I’m the guy who should be doing this?’
Yeah, I’ve been fortunate to have a couple of those ‘aha’ moments in my life. One of them was when I was an epidemic intelligence service officer back in 1998, working for the CDC in New York City. I’ve always been interested in edge issues, border issues; things that are on the boundaries between different fields. I was there in public health, but I was interested in what was happening in the rest of the world around electronic transactions and using data in a more agile way.
In disease surveillance we often look back — the way we do claims data now – years later or months later you get the reports and you look for the outbreak, and often times the outbreak’s already come and gone by the time you pick it up. But I started thinking and imagining: What if the second something happens, you can start monitoring it? In New York City the fire department was monitoring ambulance calls. I said, ‘Wow, if we could just categorize those by the type of call, maybe we’ll see some sort of signal in the noise there.’
When I was first able to visualize the trends in the proportion of ambulance dispatches in NYC that were due to respiratory distress, what I saw was flu. What jumped out at me was the sinusoidal curve. Wham! At different times of year, it could be a stutter process – it would go up and you would see this huge increase, followed two weeks later by an increase in deaths. It was like the sky opening up. The evidence was there all along, but I am the first human being on earth to see this. That was validation, for me, of the idea that electronic data opens up worlds. To bring that data to life, to be able to extract meaning from those zeros and ones — that’s life and death. That was my first ‘aha’ moment.
The second aha was after I joined New York City Department of Health, and I started a data shop to build our policy around smoking and tracking chronic diseases. What we realized was that healthcare was leaving lives on the table. There were a lot of lives we could save by doing basic stuff a third-year medical student should do, but we’re not doing it. Related to that – Tom Frieden had a great TEDMED talk about everybody counts.
I said, ‘I want to take six months off and do a sabbatical, and see if there’s anything to using electronic health records to provide those insights, not to save lives by city level, but on the 10 to the 3 level – the 1,000 patient practice. That started the whole journey. None of the vendors at the time had the vision we had, but we finally got someone to work with us and rolled this system out. We called some doctors some 23 times, and did all the work to get to the starting line. Finally, I took Tom on a field visit to see one of the first docs to get the program.
It was a very normal storefront in Harlem, and a nice physician, very caring, very typical. I asked her what she thought of the program. She said, ‘It’s ok. I’m still getting used to it.’ I said, ‘Did you ever look at the registry tab on the right, where you can make a list of your patients? She said no. I said, ok – how many of your elderly patients did you vaccinate for flu this year? She said, ‘I don’t know, about 80 to 85 percent. I’m pretty good at that.’ I said, ‘o.k., let’s run a query.’ And it was actually something like 22 percent. And she said – this was the aha moment – ‘That’s not right.’
That’s generally the feeling the docs have when they get a quality measure report from the health plan. But that’s population health management — the ability to see for the first time ever that everybody counts. And being able to then think about decision support and care protocols to reduce your defect rate. That was the validation that we’re on to something. Without the tools to do this, all the payment changes in the world can’t make healthcare accountable for cost and quality if you can’t see it.
WZ: Everyone has that moment in life when they’re considering all of their career options. As you were considering medical school, what else was on the table?
I actually didn’t think I was going to go to medical school. I was at the Harvard School of Public Health. I was interested in making an impact in public health. I grew up in Iran, and thought I would do international public health work. And then my dad got sick; he had a cardiac issue. The contrast between the immediacy of the laying on of hands of healthcare, and the somewhat abstractness of international public health — the distance, the remove — tipped me into saying, ‘You know, maybe I should go to medical school.’ I’ve been on that edge between healthcare and public health ever since, and always trying to drag the two closer to each other.
SL: Fast forward 20 years. You’re giving another talk at TEDMED. What’s the topic?
TEDMED and Jay Walker’s vision is more powerful in the futurescope, rather than in the retroscope. It’s more powerful to be where we are today and imagine a different future rather than look back and say, ‘Oh, yeah, we’ve done this.’ So what’s the future I would love to imagine?
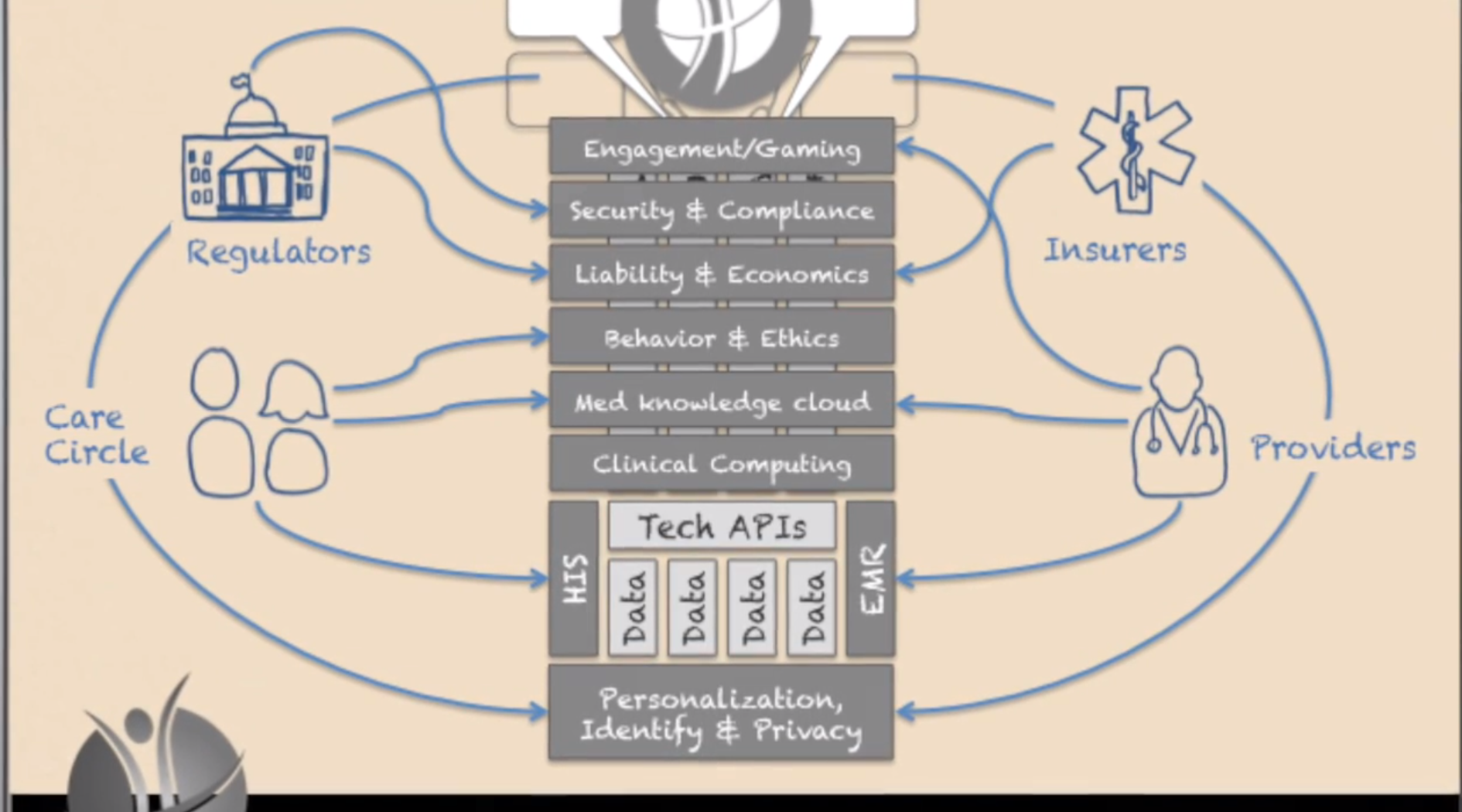
The most exciting thing – as Jay Walker once mentioned in a talk comparing “medspeed” to “techspeed” – is to fully imagine what will happen if techspeed is brought to healthcare. Right now, there’s all this unrealized value that’s being given away for free that doesn’t show up on any GDP lists – what Tim O’Reilly called “the clothesline paradox.” That kind of possibility brought to medicine, but where software costs $100,000 as opposed to free, and it evolves daily and is more powerful and quicker every day, and it’s beautiful and usable and intuitive, and that’s what people compete on.
And all of that is toward the goal of empowering people. Someone said, maybe it was Jay at TEDMED, that a 14-year-old kid in Africa with a smart phone has more access to information than Bill Clinton did as President. Information is power, and it has changed everything but healthcare. For me the vision is breaking down that wall, so that patients can be empowered and can bind themselves to the mast to use what we’ve learned about how behavior changes.
It’s not as simple as you give people information and they change their behavior. It’s information tools that build on that data and build on communities and a much more sophisticated understanding about how behavior changes. What TEDMED is also great at, is understanding the power of marketing. People think of marketing of being about advertising, but marketing is the best knowledge we have about how to change behavior and all those intangibles, those predictably irrational insights, of how and why we do what we do.
It’s harnessing those, instead of having them lead to worse health – like present value discounting that leads to people wanting to procrastinate and eat that doughnut now instead of going to the gym. Or the power of anchoring, where we fixate on the first thing we see and won’t think objectively about the true risks of things. Or the herd effect, our friend is overweight and so we are more likely to be overweight.
All those nudges that are possible can be delivered to us ubiquitously and continuously, and we can choose to have them. It’s not some big brother dystopic vision. It’s me saying, ‘I want to be healthier, so I will do something now that will help me overcome and use my irrationality to help me stay healthy. To me, that’s the neat new edge between mobile cloud computing, personal healthcare, behavioral economics, healthcare IT, data science and visualization, design, and marketing. It’s that sphere that has so many possibilities to get us to better health.
The thing about the health is, we have a Persian saying: Health is a crown on the head of the healthy that only the sick can see. When you have it, you don’t appreciate it, but when you’re sick and someone you love is sick, there’s nothing better. You would do anything to get that. We need to bring that vision of the crown to everyone and help each of us grab it when we can.
WZ: I noticed you closing your eyes while preparing to answer a question. How do you pursue being able to exercise your imagination, in particular while you’re sitting in a building that’s been marked for being the least imaginative?
Because the world, as it is, is too immediate and real and limiting, sometimes you have to close your eyes to see a different world.
What has been amazing has been to see that, contrary to what people expect, this building is filled with people with untapped, unbound, unfettered imaginations who are slogging through. They’re just trapped. You give them the opening, the smallest bit of daylight to exercise that, and they’re off and running.
I give a lot of credit to Todd Park as our “innovation fellow zero,” He saw the possibility that there are more than two kinds of people in the world, innovators and everybody else. For him, it was about going to create a space where outside innovators can be the catalyst or spark that elevates and permissions the innovation of the career civil servant at CMS in Baltimore. That’s been cool.
SL: What’s your bowtie going to do after you leave HHS? Will we see it lounging on the beach in Boca?
I like the bowtie. I think I’m going to keep it. Perhaps the @FarzadsBowtie Twitter handle is going to go into hibernation, I don’t know. I don’t control it. One of the things the bowtie does for me is help me remember not to get too comfortable.
I once said at the Consumer Health IT Summit – ‘You’re a bunch of misfits – glorious misfits. And I feel like I’m very well suited to be your leader. You know, I always felt American in Iran, and felt Iranian in America when I came here. I felt like a jock among my geeky friends, and like a geek among jocks. For crying out loud, I wear a bowtie! I don’t have to tell you I’m a misfit.’
It’s that sense of not fitting into the world as it is. The world doesn’t fit me. So instead of saying, ‘I need to change,’ this group of people said, ‘The world needs to change.’ That’s the difference between a misfit and a glorious misfit.
The person who doesn’t fit into our healthcare system is the patient. The patient’s preferences don’t fit into the need to maximize revenue and do more procedures. The patient’s family doesn’t fit into the, ‘I want to do an eight-minute visit and get you out the door’ agenda. The patient asking questions doesn’t fit. That’s the change we need to make. It’s not that we need to change. Healthcare needs to change to fit the patient.
Shortly following this interview, Dr. Mostashari left HHS and is now the a visiting fellow of the Engelberg Center for Health Care Reform at the Brookings Institution, where he aims to help clinicians improve care and patient health through health IT, focusing on small practices.
This interview was edited for length and readability.
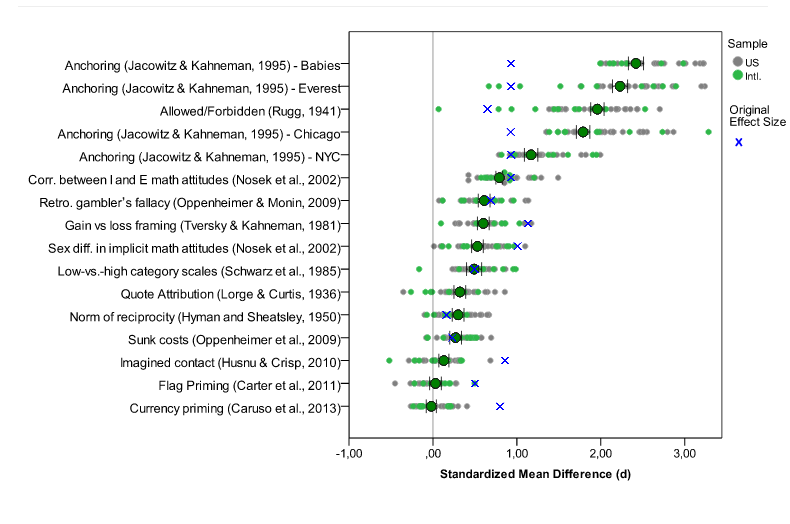 Many labs data. Blue x’s are original effect sizes. Other dots are effect sizes from replication experiments (http://rolfzwaan.blogspot.com/2013/11/what-can-we-learn-from-many-labs.html)
Many labs data. Blue x’s are original effect sizes. Other dots are effect sizes from replication experiments (http://rolfzwaan.blogspot.com/2013/11/what-can-we-learn-from-many-labs.html)

 Farzad Mostashari, MD, stepped down from his post as the National Coordinator for Health Information Technology at the U.S. Department of Health and Human Services (HHS), during the first week of October, which was also the first week of the Federal partial shutdown. During his tenure, Dr. Mostashari, who
Farzad Mostashari, MD, stepped down from his post as the National Coordinator for Health Information Technology at the U.S. Department of Health and Human Services (HHS), during the first week of October, which was also the first week of the Federal partial shutdown. During his tenure, Dr. Mostashari, who