The American economist William A. Niskanen considered the organisation of bureaucracies and proposed a budget maximising model now influential in public choice theory. It stated that rational bureaucrats will “always and everywhere seek to increase their budgets in order to increase their own power.”
An unfettered bureaucracy was predicted to grow to twice the size of a comparable firm that faces market discipline, incurring twice the cost.
http://theconversation.com/reform-australian-universities-by-cutting-their-bureaucracies-12781
Reform Australian universities by cutting their bureaucracies

Universities drive a knowledge economy, generate new ideas and teach people how to think critically. Anything other than strong investment in them will likely harm Australia.
But as Australian politicians are preparing to reform the university sector, there is an opportunity to take a closer look at the large and powerful university bureaucracy.
Adam Smith argued it would be preferable for students to directly pay academics for their tuition, rather than involve university bureaucrats. In earlier times, Oxford dons received all tuition revenue from their students and it’s been suggested that they paid between 15% and 20% for their rooms and administration. Subsequent central collection of tuition fees removed incentives for teachers to teach and led to the rise of the university bureaucracy.
Today, the bureaucracy is very large in Australian universities and only one third of university spending is allocated to academic salaries.

Across all the universities in Australia, the average proportion of full-time non-academic staff is 55%. This figure is relatively consistent over time and by university grouping (see graph below).
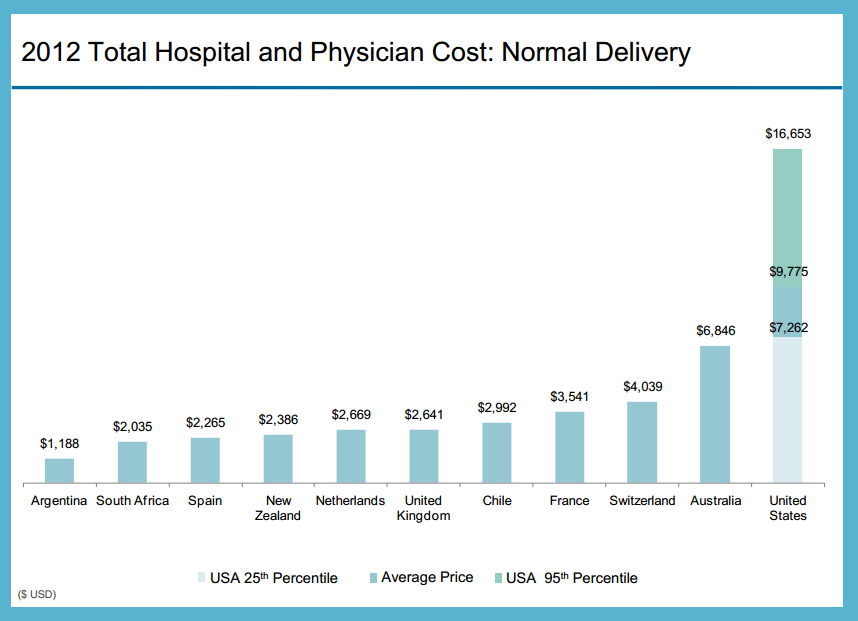
Australia is not alone as data for the United Kingdom shows a similar staffing profile with 48% classed as academics. A recent analysis of US universities’ spending argues:
Boards of trustees and presidents need to put their collective foot down on the growth of support and administrative costs. Those costs have grown faster than the cost of instruction across most campuses. In no other industry would overhead costs be allowed to grow at this rate – executives would lose their jobs.
We know universities employ more non-academics than academics. But, of course, “non-academic” is a heterogeneous grouping. Many of those classified as “non-academic” directly produce academic outputs, but this rubs both ways with academics often required to produce bureaucratic outputs.
An explanation for this strange spending allocation is that academics desire a large bureaucracy to support their research efforts and for coping with external regulatory requirements such as the Excellence in Research for Australia (ERA) initiative, theAustralian Qualifications Framework (AQF) and the Tertiary Education Quality and Standards Agency (TEQSA).

Another explanation is that university bureaucracies enjoy being big and engage in many non-academic transactions to perpetuate their large budget and influence.
The theory to support the latter view came from Cyril Northcote Parkinson, a naval historian who studied the workings of the British civil service. While not an economist, he had great insight into bureaucracy and suggested:
There need be little or no relationship between the work to be done and the size of the staff to which it may be assigned.
Parkinson’s Law rests on two ideas: an official wants to multiply subordinates, not rivals; and, officials make work for each other. Inefficient bureaucracy is likely not restricted to universities but pervades government and non-government organisations who escape traditional market forces.
Using Admiralty Statistics for the period between 1934 and 1955, Parkinson calculated a mean annual growth rate of spending on bureaucrats to be 5.9%. The top ten Australian research universities between 2003 and 2010 report mean annual growth in spending on non-academic salary costs of 8.8%. After adjusting for inflation the annual growth rate is 5.9%.
The American economist William A. Niskanen considered the organisation of bureaucracies and proposed a budget maximising model now influential in public choice theory. It stated that rational bureaucrats will “always and everywhere seek to increase their budgets in order to increase their own power.”
An unfettered bureaucracy was predicted to grow to twice the size of a comparable firm that faces market discipline, incurring twice the cost. Some insight and anecdotal evidence to support this comes from a recent analysis of the paperwork required for doctoral students to progress from admission to graduation at an Australian university.
In that analysis, the two authors of this article (Clarke and Graves) found that 270 unique data items were requested on average 2.27 times for 13 different forms. This implies the bureaucracy was operating at more than twice the size it needs to. The university we studied has since slimmed down the process.
Further costs from a large bureaucracy arise because academics are expected to participate in activities initiated by the bureaucracy. These tend to generate low or zero academic output. Some academics also adopt the behaviour of bureaucrats and stop or dramatically scale back their academic work.
The irony is that those in leadership positions, such as heads of departments, are most vulnerable, yet they must have been academically successful to achieve their position.
Evidence of this can be seen from the publication statistics of the professors who are heads of schools among nine of the top ten Australian research universities. Between 2006 and 2011, these senior academics published an average of 1.22 papers per year per person as first author.
This level of output would not be acceptable for an active health researcher at a professor, associate professor or even lecturer level.
The nine heads of school are likely tied up with administrative tasks, and hence their potential academic outputs are lost to signing forms, attending meetings and pushing bits of paper round their university.
If spending on the costs of employing non-academics could be reduced by 50% in line with a Niskanen level of over-supply, universities could employ additional academic staff. A further boost to productivity could be expected as old and new staff benefit from a decrease in the amount of time they must dedicate to bureaucratic transactions.
If all Australian universities adopted the staffing profile of the “Group of 8” institutions, which have the highest percentage of academics (at 51.6%), there would have been up to nearly 6,500 extra academics in 2010.
While no economist would question the need for some administration, there needs to be a focus on incentives to ensure efficient operation. It’s possible to run a tight ship in academic research as shown by Alan Trounson, president of the California Institute for Regenerative Medicine (CIRM).
In 2009, Trounson pledged to spend less than 6% of revenues on administration costs, a figure that is better than most firms competing in markets. So far, this commitment has been met.
It’s clear then that finding solutions to problems in modern Australian universities calls for a better understanding of economics and a reduction in bureaucracy.
 Graphic
Graphic