http://www.iedp.com/Blog/Ten-Predicaments-Facing-a-New-CEO
|
||
10 Predicaments Facing a New CEO |
||
|
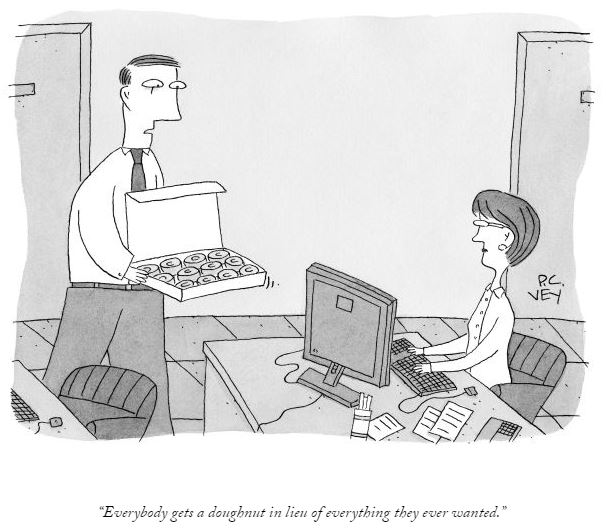
Finally the day arrived, when Peter was appointed as the CEO of the multinational technology giant. After months of speculation, apprehension and expectation; all came to a logical conclusion and everyone sighed with relief. Stakeholders were satisfied, the board were confident of having made the right choice, and the outgoing CEO felt that he was leaving the company in safe hands. When a week long ceremony and celebrations were over, Peter got some reflective moments to himself. That night, he could not sleep. He wondered, ‘what next’? Where does he go now, from here onward? Who to look up to, where to escalate and where does the buck stop now? Unfortunately, the buck now stops with him. Peter knew that from now onwards, everybody including customers, stakeholders, employees, the market and board will look to him for direction; looking for those ‘Pearls of Wisdom’ that he had been craving to apply or holding on to reveal now that he had reached this stage. This a usual scenario in most companies, where succession has happened or is likely to happen in the near future. CEOs are always in the ‘Hot Seat’, irrespective of whether their businesses are struggling due to competition, context or capability; or doing exceptionally but where the continual drive for aspirational growth continues. They have to deal with a number of predicaments that put a strain on their time, energy and decision making. Either way, here are 10 top dilemmas new CEOs will do well to know in advance and brace their organizations to deal with effectively:
Finding business coherence amidst the randomness of internal and external events is a perpetual dilemma for the CEOs. A lot will depend upon, how he marshals his resources in new and innovative ways to discover that elusive growth orbit for which he has been appointed as the CEO. Discovering new ways of value creation and building conviction around them will help him deal with above predicaments, effectively. Each and every dilemma must be dealt with a filter of Staying Relevant – Proactive Disruption and Building case for Strategic Change. Finally, not everyone will understand the path undertaken by CEO but as long as these paths enable him and the company ‘Stay Relevant’ to its customers, they must be pursued with conviction. Illustration: King Arthur. Fresco (detail) in the Corridor, Trinci Palace, Foligno, Italy Further Information
|

 VIEWPOINT: No career move is more profound than the step up to CEO.
VIEWPOINT: No career move is more profound than the step up to CEO. 

 Himanshu Saxena is a thinker, writer and speaker on concepts such as Big Picture, Reimagination, Strategy & Innovation and Leadership@Top Level. He is currently enabling TCS BPS in aligning strategy, coaching and developing leaders of tomorrow.
Himanshu Saxena is a thinker, writer and speaker on concepts such as Big Picture, Reimagination, Strategy & Innovation and Leadership@Top Level. He is currently enabling TCS BPS in aligning strategy, coaching and developing leaders of tomorrow. Vijay Govindarajan is the Coxe Distinguished Professor at the Tuck School at Dartmouth and the author of NYT and WSJ Best Seller, Reverse Innovation.
Vijay Govindarajan is the Coxe Distinguished Professor at the Tuck School at Dartmouth and the author of NYT and WSJ Best Seller, Reverse Innovation.