Upper endoscopies may bilk Medicare
http://www.forbes.com/sites/peterubel/2014/05/22/are-gastroenterologists-scoping-for-dollars-on-medicare-patients/
5/22/2014 @ 11:23AM |801 views
Inappropriate Medicare Incentives Lead To Unnecessary Subspecialty Procedures
Sometimes people flat out need cameras shoved down into their stomachs. A long history of reflux disease, for example, could prompt a gastroenterologist to perform an “upper endoscopy”—to run a thin tube down the patient’s throat in order to view their esophagus and stomach and look for signs of serious illness. Medicare has correctly decided that such upper endoscopies are valuable medical tests, and reimburse physicians relatively generously for performing them. But what should Medicare do when gastroenterologists unnecessarily repeat these tests in patients who do not show signs of serious illness on their first exam?
I became aware of this issue after reading an article in the Annals of Internal Medicine by Pohl and colleagues. Pohl glanced at billing data from a random sample of almost 1 million Medicare enrollees. (I am pleased with myself when I pull together a study of a few hundred patients. Perhaps I won’t be so pleased in the future.)
Pohl and colleagues analyzed how many patients received more than one upper endoscopy within a three year period. They then tried to figure out how often these repeat procedures were necessary, because of abnormalities discovered in the initial exam.
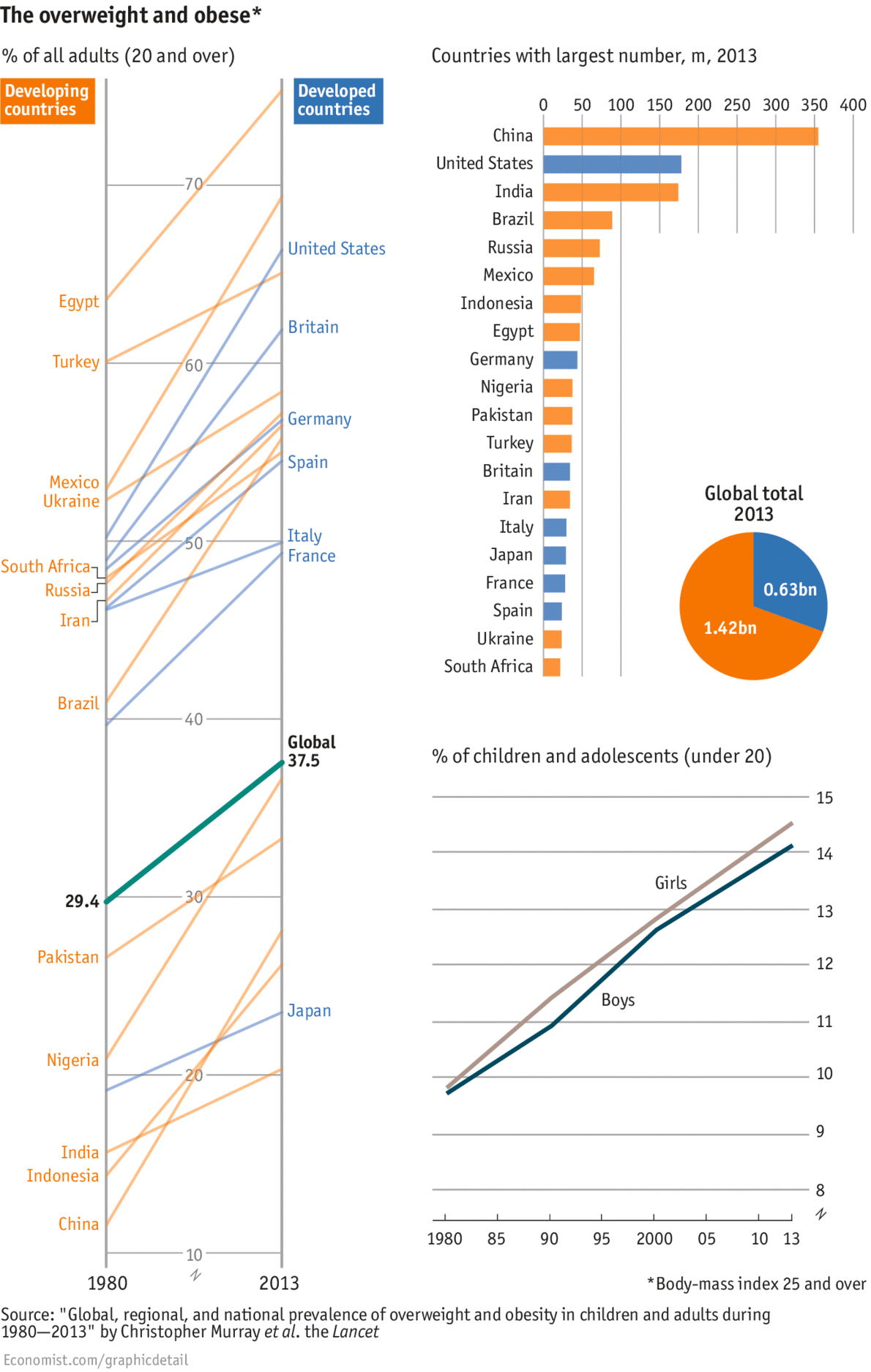
Let’s start with the bad news. Among those patients who should have received repeat tests, only half did so. That means even when doctors found bad things that needed to be followed up, it was practically a flip of a coin whether they would do so.
Now for the worse news. Among those who should not have received a follow-up test, a full 30% did, for a total of 20,000 such tests in this population. Here is a picture summarizing the results:

Here is another way to look at these results. Among patients receiving upper endoscopies, the majority –54%—should not have received these tests.
Now for some back-of-the-envelope math. The sample of patients Pohl and colleagues looked at made up 5% of the Medicare population. That means if you take their estimates of how many gastroenterologists performed unnecessary upper endoscopies over the three year period of their study, and multiply that estimate by 20, you end up with 4 million unnecessary endoscopies nationwide. With the average costs of such a procedure being around $3,000, that amounts to $1.2 billion of our tax dollars wasted on an unnecessary and, I should mention, uncomfortable and potentially harmful procedure. (Warning: I don’t know what Medicare pays for this test. But we are still talking hundreds of millions of dollars, in a best case scenario.)
In an editorial accompanying the Annals study, a gastroenterologist bemoaned these unnecessary procedures and recommended several steps we could take to reduce such testing. First, the editorialist said we should help physicians better understand when they should and should not use such procedures. Second, he said we “must also educate patients about the modest yield” of such tests.
I find this last idea…what’s a nice way to put this…highly naïve. (Haive?)
What we need to do is to stop paying doctors for unnecessary tests. Or alternatively, we need to pay doctors in ways that reduce their incentive to perform unnecessary tests, like lump sums to take care of all of their patients’ needs.
While some gastroenterologists may be cynically scoping patients for dollars—performing questionable tests because it pays for their kid’s private school tuition—I expect most believe such testing is in their patient’s best interests. We need an incentive system that forces them to think more carefully about when—or whether—these expensive tests are necessary.