in reference to the green’s attempt to include the casino in the Barry O’Farrell alcohol fuelled violence crackdown
Category Archives: storytelling
Menadue on Medicare on its 40th anniversary
A terrific insider account of the extremely organic conception and birthing of Medicare (nee Medibank)….
John Menadue. 30th anniversary of Medicare
Feb 1 is the 30th anniversary of Medicare. But the story of Medicare really goes back 40 years to the passing of the Medibank legislation by the Whitlam Government in a joint session of the Parliament on 7 August, 1974.
Medibank started on schedule on 1 July 1975 when health insurance cards were issued to the Australian population.
But the Fraser Government attempted to wind back Whitlam’s Medibank. The Fraser Government introduced legislation for Medibank Mark 2 that included a 2.5% levy and gave the public an option of taking out private insurance instead of paying the levy. It established Medibank Pte.
On 1 Feb 1984, the Hawke Government re-established the basic design of Whitlam’s Medibank. There were financial changes and the name changed from Medibank to Medicare which we have today.
Medibank/Medicare was always a public insurance scheme. It has never delivered health services. It financed the existing health ‘system’. Unfortunately in the days since the establishment of Medibank/Medicare the health “system” has not been seriously reformed to reflect the experience and the needs of today. The vested interests in the health system that tried so desperately to derail Medibank/Medicare over a long period are still in play today, holding back essential reform.
I wrote the article which is reproduced below in July 2000. It was published in the Medical Journal of Australia. It sets out the long and difficult struggle to launch Medicare.
Down a different path in Melbourne: how Medibank was conceived (John Menadue)
On a bleak midwinter night, the germ of an idea crystallised into a grand plan.
It was hard-going developing policies in Opposition, particularly for a reform party out of power during the long Menzies ascendancy. The task was made harder in Australia, with our written Constitution interpreted for many years by a conservative High Court.
A historic meeting
Health policy was no exception, but a turning point came on the night of 6 June 1967, at the home of Dr Moss Cass in Melbourne. Cass was among the most farsighted and perceptive thinkers on health policy that I have met. Cass was then in charge of a trade union health clinic in Melbourne and later became a Minister, but not Health Minister, in the Whitlam governments.
As Gough Whitlam’s Chief of Staff in an office of only three people in the mid-1960s, I had been building up groups of people who could advise him on a range of issues, such as education, science, housing, transport and health. These groups were the building blocks that Whitlam used to rewrite almost the whole of the ALP (Australian Labor Party) platform. That work came to fruition in the ALP’s election victory of 1972. The groups were made up of professionals, academics and other reform-minded people who freely gave their skill and time. Few were members of the ALP.
Professor Sol Encel was my chief collaborator in building these groups. He was Reader in Political Science at the Australian National University at the time and later became Professor of Sociology at the University of New South Wales. Encel suggested Cass as an adviser on health policy. Cass had written an influential Fabian Society pamphlet on health policy and advocated a national health system founded on public hospitals and health centres staffed by salaried doctors.
In 1967, the ALP’s election prospects seemed as bleak as the midwinter night when Whitlam and I rang Cass’s front door bell. Many years later, Whitlam asked me what time of the year the meeting was held. I recalled it was midwinter because Cass had lit a log fire to try to cheer us up. The evening turned out to be a historic turning point, although no-one recognised it at the time. If we had realised how important it was, we would at least have had a photographer present!
Cass had also invited Dr Rod Andrew, Foundation Dean, Faculty of Medicine at Monash University, who had been a public advocate of more salaried staff in hospitals. Also present was Dr Jim Lawson, Superintendent of the Footscray Hospital, who was described by Cass as having a view that there were too many hospital beds, and that they should be used more efficiently and with greater emphasis on care in the community. Dr Harry Jenkins, the ALP spokesman on health in the Victorian State Parliament, was also present. However, the key attendees. were two young researchers from the Institute of Applied Economic Research at Melbourne University, John Deeble and Dick Scotton. Deeble had previously been Deputy General Manager of the Peter MacCallum Clinic in Melbourne. Scotton had been economist at the Commercial Banking Company in Sydney and doing ground-breaking research at Melbourne University on the pharmaceutical industry, hospital costs and compulsory and voluntary health insurance.
A scheme of universal health insurance
From that 6 June 1967 meeting, Deeble and Scotton developed a universal and compulsory health insurance scheme to be funded by a tax levy. It was clear that the Liberal-Country Party Coalition Government’s voluntary health insurance scheme, supported by taxpayers’ funds, was wasteful and inequitable and that an alternative was needed.
In May 1968, Deeble and Scotton distributed their paper, A scheme of universal insurance (unpublished paper, Institute of Applied Economic Research, May 1968). Whitlam used this academic treatise as a major input in his own policy development. In July that year, 13 months after the meeting at Cass’s house and almost five years before he became Prime Minister, Whitlam outlined The alternative national health program (called “Medibank”, and later “Medicare”), which was to become so much part of Australian national life. The Deeble and Scotton ideas became a practical and political program. Once again, rigorous policy development and a compelling Whitlam speech became party policy.
In retrospect, the June 1967 meeting took health down a path that neither Whitlam nor I expected. We were looking in another direction. Medibank was about financing access to “the health system”, not about how the health system could better deliver services to the community. It is noteworthy that, 25 years after the obvious success of Medibank, with increased demands on the health system in a consumer society, we are being forced to again consider how we can better deliver health services. Access to “the health system” is no longer sufficient; the system itself needs attention.
In most of the seven years I spent with Whitlam, we were not working on a compulsory health insurance scheme, but focusing on how to develop and strengthen a public hospital system with regional clinics and services. Because of the constitutional and political barriers to nationalisation of the medical profession, the only feasible route seemed to be via increased Federal Government funding for expanded State public hospital systems that could compete with private hospitals and private doctors.
The overseas experience
Many of us in the ALP at the time were attracted to the National Health Service (NHS) which the British Labour Party had introduced in the 1940s. But such a scheme in Australia was constitutionally impossible. It was also politically hazardous, with doctors in many countries suspicious of and rigorously opposed to the British NHS at the time, although it has stood the test of time much better than its many critics.
With Cass’s assistance, we read the literature on different healthcare schemes around the world. What caught our attention were the many surveys and analyses which showed that fee-driven, private medicine resulted in excessive treatment, high costs and orientation away from preventive care. These health schemes were overwhelmingly producer- rather than consumer-driven and were inherently unstable, with suppliers of the services substantially managing the demand. I recall particularly articles in the New England Journal of Medicine about the development of health maintenance organisations in the United States in response to escalating private health costs.
A national hospital system
In 1961, long before Deeble and Scotton came along and Medibank was conceived, Whitlam had described his path for health reform in his Curtin Lecture: “…the best way to achieve a proper national health service is to establish a national hospital system.” He added:
“…the proper approach is for the Commonwealth to make additional grants to the States on condition that they regionalise their hospital services and establish salaried and sessional medical and ancillary staff in hospitals.”
These ideas were further developed and articulated in a speech which he gave to the citizens of Rochester, Victoria, in 1964. They were clearly nonplussed when, at their rural hospital, he told them that “it is more important to nationalise hospitals than to nationalise the medical profession”. What was he talking about? This was Whitlam’s way of circumventing the constitutional obstacles, although it seemed very remote from the problems facing Rochester. While Federal Parliament could “make laws with respect to … pharmaceuticals, sickness and hospital benefits”, it could not “authorise any form of civil conscription”. Nationalisation of the medical profession, as in the United Kingdom, was out, but a national health service based on “Section 96″ federal grants to the States for hospitals with regional health services and employing salaried staff was seen as a way forward. There would be choice for doctors and patients. (Under Section 96 of the Australian Constitution, “the [Commonwealth] Parliament may grant financial assistance to any State on such terms and conditions as the Parliament thinks fit”.)
Elected in 1972, the Whitlam Government introduced a five-year program of capital assistance for hospitals. Under Section 96 of the Constitution, these were “special purpose grants”. The Fraser* Coalition Government did not renew the program, nor did the Labor governments of Hawke or Keating.
However, after June 1967, major health reform was to go down the Medibank compulsory insurance route rather than the funding of hospitals and related services. Medibank would prove simpler to explain and implement. It was also a more likely political winner.
Voluntary versus compulsory health insurance
While developing reforms based on hospitals, Whitlam had been persistently criticising the shortcomings of voluntary health insurance. He had asked many questions on notice in Federal Parliament since the early 1960s about the high cost, high reserves and limited coverage of private health funds. We were of the view that, on a per capita basis, the total cost of the Australian health system exceeded by a large margin the cost of the NHS in the United Kingdom, but we were finding it hard to prove. We could identify the Government’s health costs, but the additional costs to individuals, either directly or through their health funds, were hard to pin down. We suspected that the higher costs in Australia were due to the inefficiencies of the health funds and the perverse financial incentives inherent in fee-for-service, which encouraged over servicing and overprescribing.
So when Whitlam met Deeble and Scotton to discuss their new approach to health insurance, he was very receptive, although I recall that the 6 June meeting was slow to begin, with Whitlam’s eyelids drooping a few times. But his interest sparked up dramatically when Deeble and Scotton explained that in their view a compulsory and universal scheme would be cheaper than existing arrangements. There· was thus the exciting prospect ahead of a health scheme that was both universal and also politically defensible as to its cost.
Whitlam’s critique of voluntary health insurance, supported by the work of Deeble and Scotton, was confirmed by Justice Nimmo in his 1969 report. (The Coalition Government had established the Nimmo inquiry into health insurance to try to pre-empt the findings of a Senate committee which was reviewing health insurance.)
The campaign against Medibank
The long drawn out battle for the Medibank reforms was unrelenting in both the 1969 and the 1972 elections. John Cade, General Manager of the Medical Benefits Funds of Australia, said in August 1968, one month after Whitlam outlined his “Alternative National Health Program”, that “Karl Marx’s theories have never been wanted by Australians in the past and they are needed even less today …If you want to pervert the truth and have it believed, tell a whopper and tell it often!”
It wasn’t a particularly well argued or dispassionate analysis of Whitlam’s proposals, but Cade’s comments give some idea of the hype and passion of the anti-Medibank campaign. Health funds spent contributors’ money, including mine, to fight Medibank.
The Australian Medical Association (AMA) and the more militant General Practitioners’ Society in Australia conducted a shrill and long campaign against Medibank. An AMA “freedom fund” was established. Television, radio and newspaper advertising, supported by a public relations campaign, was waged relentlessly, year after year. The AMA sent letters and publicity kits to all doctors. They were designed to keep up the “noise level”. Even a former Miss Australia was called to the battlefront following petitions in Federal Parliament and “calls to action” by doctors. Without any apparent sense of irony, the campaign against Medibank was described by the AMA as protecting the “doctor and patient relationship”.
The two Medibank Bills were three times rejected by the Senate after the 1972 election and were only finally passed after a double dissolution of Federal Parliament and the joint sitting of Parliament in July 1974. The Medibank Bills were two of the six Bills on which a double dissolution had been secured in April 1974. But, even then, the Coalition Opposition, supported by doctors, would not concede. The implementation of Medibank was delayed further by the Senate in late 1974 when it rejected three Bills to impose a 1.35% levy on taxable incomes. As a result it was decided to finance the scheme initially from general revenue, and the funding was provided in Bill Hayden’s first Budget in August 1975. At that time I was Secretary of the Department of Prime Minister and Cabinet.
The future
It had been a long and bitter campaign from that midwinter night in Melbourne in 1967 to spring in Canberra in 1975. No government will now seriously tamper with the compulsory and universal health insurance scheme. The area of concern and debate for the future will not be so much about funding of Medicare, but rather about how we improve the delivery of health services.
Meryl Streep: It’s bizzarre that the Produce Manager is more important to my children’s Health than the pediatrician.
Fear + Clear Action = Effective Behaviour Change
- people indulge in unhealthy behaviours to relieve stress and anxiety
- ads that cause stress and anxiety can drive unhealthy behaviours
- one solution is to couple compelling threats with clear and specific paths to behaviour change
- another approach is to apply the adicitive rewards that video games create for real life challenges
- SUPERBETTERLABS.COM build video games which build resilience and maintain motivation while working to overcome injuries, anxiety and depression
http://www.iodine.com/blog/anti-smoking-ads/
Why Graphic Anti-Smoking Ads Make Some People Smoke More Cigarettes
Jessica Goldband
If these images make you squirm or want to click away, you’re not alone.
How, then, can this type of message change the choices you make? Can we really be motivated by something that turns us off, rather than on?
You’d think, perhaps intuitively, that the scarier the ad, the more powerfully it affects our behavior. And the research supports that argument. Indeed, since the classic 1964 Surgeon General report on “Smoking and Health” came out 50 years ago this month, that’s been the basic strategy for health communication around the issue. But there’s a catch. A BIG one.
While we’ve seen a significant drop in global smoking rates (down 25% for men and 42% for women) since those landmark reports in the 1960s demonstrated the link between smoking and lung cancer, many people continue to smoke: 31% of men and 6% of women. In the U.S., 18% of adults (down by half since 1964) continue to do something they know might kill them.
Public health agencies have spent years communicating the dangers of smoking. Their anti-smoking ads have grown increasingly disturbing, threatening us with graphic images of bulging tumors and holes in our throats — possibly to try to reach that last stubborn segment of the population that hasn’t kicked the habit.
Why aren’t these ads working?
Turns out, the most recent and comprehensive research on so-called “fear appeals” and attitude change says that this kind of messaging does work, but only if the person watching the ad is confident that they are capable of making a change, such as quitting smoking. Public health gurus call this confidence in one’s ability to make a change “self-efficacy” — and threats only seem to work when efficacy is high. (The reverse is also true.)
If someone lacks efficacy, ads with fear appeals don’t help. In fact, they make the behaviorworse. How? Many people engage in unhealthy behavior because it makes them feel better and relieves their anxiety.
If you threaten someone who has little to no confidence they can change their behavior, their anxiety goes through the roof. What do they do? Perhaps turn off the threatening ad, walk away, and light up a cigarette — the very behavior you were trying to prevent. This same principle applies to other coping behaviors, such as eating unhealthy types of food or just too much of it.
Unfortunately, anxiety is quite common in this country. According to arecent Atlantic article, 1 in 4 Americans is likely to suffer from anxiety at some point in life. Making big life changes is tough, and it seems as though fear and anxiety don’t energize people, they just paralyze them.
So what’s the solution?
A step in the right direction would be for ad campaigns to couple compelling threats with equally clear and specific paths to behavior change. Or why not apply the rewards built into reaching a new level in addictive video games to apps that people can use for real-life challenges? One great example of this is Superbetter, a social online game to help people build resilience and stay motivated while working to overcome injuries, anxiety, and depression.
Stand-alone threats implicitly assume that people don’t already know how bad their choices are, and can drive them to the very behaviors they wish they could change. Truly effective ad campaigns might still appeal to our fears, but they should also let us wash it all down with a confidence chaser that empowers the more anxious among us to act on our fears.
Katz smashes it again… it’s the culture, stupid.
“Bariatric surgery is effective and should be available to those who need it. I have referred patients for such surgery over the years. But our culture will be defined by what we learn and share. We could learn and share the skill set for losing weight and finding health, and make that our cultural norm.”
…but how do we operationalise culture change…. it is massive task, but it needs to happen. Purpose perhaps?
Obesity and Oblivion- or- What I’ve Learned Under General Anesthesia

I am going to tell you what I’ve learned under general anesthesia, but I ask you to bear with me kindly and wait a few paragraphs for that revelation.
I am a rambunctious guy, pretty much always have been. I have always loved active recreation and was one of those kids who had to be reeled in for dinner from outside play with a winch and a cable. As an adult, I placate the restlessness of my native animal vitality with about 90 minutes of exercise every day. In addition, I hike whenever I can, and pretty much share my dogs’ attitude about it: the more miles, the better. I studied the martial arts for years. I am a lifelong, avid alpine skier, and an ardent equestrian– privileged to share that latter brand of rambunctiousness with my beautiful horse, Troubadour, who seems to enjoy running and jumping as much as I do, and is far better at it.
This is all part of family tradition. Women in the family are generally quite active, and some have their share of perennial restlessness. But the guys are a case apart. My son’s rambunctiousness is, quite literally, famous of song, story, and program. The ABC for Fitness™ program Gabriel directly inspired is now reaching hundreds of thousands of kids around the country and world, and paying forward the benefits of daily exercise in schools. Gabe helped me appreciate the importance of asserting that the proper remedy for rambunctiousness in our kids is recess, not Ritalin.
And then there’s my father, whose restlessness is the granddaddy of all, and the stuff of legend, or at least family lore. We celebrated his 74 birthday last summer with a hilly, 56-mile bike ride.
By and large, the effects of this rambunctiousness are extremely positive. My animal vitality is spared the constraints of leash or cage, and rewards me reciprocally with energy, stamina, and productivity. But everything has a price. My particular brand of rambunctiousness has involved pushing limits, and limits have a tendency of pushing back. The result is several concussions (I am now a consistent helmet wearer), too many stitches to count, roughly 20 broken bones, and general anesthesia to restore the mangled anatomy of some joint or other not fewer than a half dozen times.
Which leads, at last, to what I’ve learned under general anesthesia: Nothing. Nada. Zip.
Nobody learns anything under general anesthesia. General anesthesia involves unconsciousness; oblivion.
And on that basis, I consider it a societal travesty that hyperendemic obesity and the metabolic mayhem that often follows in its wake are treated ever more frequently, in ever younger people, under general anesthesia. Our answer to obesity is, it seems, oblivion.
True, bariatric surgery is effective. But it is also expensive, and subject to all of the potential complications of surgery. We don’t really know how long the benefits last, particularly for the children and adolescents who are candidates in growing multitudes. We do know that lasting benefit requires ancillary lifestyle change, and that there is often some, and sometimes a lot, of weight regain despite the rewiring of the gastrointestinal tract.
And we know as well that we are relying on scalpels in the hands of others to do what forks in our own hands (and feet in our own shoes) could do better, at dramatically lower cost and risk, if our society committed to empowering their more salutary use. We have evidence to suggest that schools and aptitudes acquired there could do for weight what scalpels applied under anesthesia do. But in my experience, they could do so much more. As a medical advisor at Mindstream Academy, a boarding school producing weight loss to rival bariatric surgery, I have been far more impressed with what the kids find than what they lose, impressive though the latter may be. They find pride and proficiency; confidence and competence; skillpower and self-esteem. They learn, in other words- as nobody ever does under general anesthesia.
Our society’s tendency to “over-medicalize” has been chronicled by others. The consequences extend to expecting from our clinics what only our culture can deliver. Among the most vivid illustrations of this is the lifelong work of my friend, Dean Ornish. Dr. Ornish was involved in groundbreaking work that showed the capacity for a lifestyle overhaul to rival the effects of coronary bypass surgery. With evidence in hand that feet and forks (and a short list of other priorities attended to) could do for coronaries what scalpels could do, Dr. Ornish set out to make his lifestyle program a reimbursable alternative to surgery. He succeeded, earning Medicare reimbursement after – wait for it- 17 years! I don’t know that Dean has the patience of a saint, but he apparently does have the patience of a cicada.
It took 17 years to gain reimbursement for lifestyle as a cost-effective treatment of coronary artery disease, whereas surgery was reimbursed from the get-go. That’s how we roll, and then wring our hands about the high costs of health care.
With that in mind, I ask my fellow parents reading this column; I ask the grandparents, godparents, aunts and uncles to contemplate this: How many of our sons and daughters, nieces, nephews, and grandchildren will have passed through the O.R. doors if it takes us two decades to establish lifestyle intervention as a culturally sanctioned alternative to bariatric surgery? However many that is, I can tell you exactly what they will all learn while under general anesthesia: Nothing. Nada. Zip.
Knowledge and experience are the foundational elements of culture itself. Culture derives from the capacity of our species to learn, and pay forward our learnings to our contemporaries and our children. Among the impressive manifestations of effective school-based approaches to adolescent obesity is the capacity, and proclivity of the kids to pay their newly acquired skillpower forward. When last I visited Mindstream Academy, one of the young girls there, who had lost some 80 lbs, was most proud to tell me about her father back at home who, courtesy of her long-distance coaching, had lost about 40. There is nothing to pay forward following the oblivion of general anesthesia.
Bariatric surgery is effective and should be available to those who need it. I have referred patients for such surgery over the years. But our culture will be defined by what we learn and share. We could learn and share the skill set for losing weight and finding health, and make that our cultural norm. That remains unlikely so long as we put our money preferentially where our medicalizations are. The AMA has proclaimed obesity a disease, but that’s just symptomatic of our culture tendencies. It is more a disease of the body politic than of the often healthy bodies that succumb to it in a culture that propagates its causes.
The healthiest, happiest, leanest, longest-lived populations on the planet do not attribute such blessings to the proficiency of their surgeons or the frequency of their clinical encounters. They attribute them to the priorities and prevailing norms of their culture.
Nobody learns anything under general anesthesia. General anesthesia is oblivion. If we keep prioritizing the medical over the cultural, oblivion over enlightenment, my friend Dean Ornish will remain a lonely pioneer. And the cicadas, when next they emerge, will see nothing new. They will have cause to roll their protuberant eyes at us and trill out: same as it ever was.
It doesn’t have to be that way. We could choose oblivion a bit less often, and stay conscious instead. Conscious, we would have a chance to think outside the box of surgical gloves- and perhaps thereby perceive a new world of opportunity.
-fin
Dr. Katz was recently named one of the most influential people in Health and Fitness (#13) byGreatist.com. His new book, DISEASE PROOF, is available in bookstores nationwide and at:
Dr. David L. Katz; www.davidkatzmd.com
www.turnthetidefoundation.org
http://www.facebook.com/pages/Dr-David-L-Katz/114690721876253
http://twitter.com/DrDavidKatz
http://www.linkedin.com/pub/david-l-katz-md-mph/7/866/479/
DH getting serious on healthy food policy
- getting rid of guilt lanes at supermarket checkouts
- removal of confectionery and soft drinks from gondola ends
- voluntary code to limit marketing (incl. use of cartoon characters) of HFSS to children
- Lidl trials of juices and fresh fruit in checkouts attracted 20% higher footfall
- a new pilot scheme in a Morrisons store in Salford, using cardboardboard cut-outs of local GPs in the fresh produce aisles delivered a 20% rise in the sales of fresh fruit and a 30% uplift for frozen fruit.
Tip: http://www.foodpolitics.com/2014/01/how-to-get-people-to-buy-healthier-food-cardboard-cutouts/
DH wants new Responsibility Deal measures to tackle unhealthy food promotions

Cardboard cut-outs of local GPs convinced Salford shoppers to buy 20% more fresh fruit
The government has given retailers and suppliers a “short window of time” to agree a voluntary clampdown on the promotion of foods high in fat, salt or sugar as it prepares to launch a new strategy to fight childhood obesity in the spring.
The DH claims supermarkets and suppliers can supply the final piece in the jigsaw in its Responsibility Deal if they support a raft of proposals, including getting rid of “guilt lanes” at checkouts and the removal of sweets and sugary fizzy drinks from gondola ends. It is also planning a new voluntary code to limit the marketing of HFSS products to children. Talks before Christmas between health secretary Jeremy Hunt, health minister Jane Ellison and CEOs of suppliers and all the major supermarkets focused on protecting children from obesity and Ellison said she was “hopeful” they would result in a “package of measures”. Dr Susan Jebb, chair of the Responsibility Deal food network, who was central to the talks, said: “We’ve challenged them to think what they might do from a long and wide-ranging list of ideas. We’re giving the industry a short window of time to come back with a response.” She said pressure was growing on the government to regulate if companies failed to respond to the calls. With pressure on the DH reaching fever pitch in the wake of this week’s alarmist reports, it wants a commitment to guarantee a minimum level of price and loyalty promotions for healthier options, the banning of cartoon characters on packaging of HFSS foods and restrictions on online promotions. This week, discounter Lidl promised to roll out its ‘Healthy Checkouts’ concept – an initiative first trialled last year – replacing unhealthy items with fresh fruit and juices at tills, claiming the trial stores attracted a 20% higher footfall. “I think it’s a bold move,” said Jebb. “What I find very encouraging is that they’ve done it in response to what their customers want and I think it sends a powerful message to other retailers.” “This is a huge opportunity for the industry to show that a voluntary strategy is the way to deal with the obesity crisis,” she added. “We’re tackling satfats, calories and salt, and the thing that would wrap it all up is something around promotions.” Meanwhile it was revealed this week that a new pilot scheme in aMorrisons store in Salford, using cardboardboard cut-outs of local GPs in the fresh produce aisles delivered a 20% rise in the sales of fresh fruit and a 30% uplift for frozen fruit.
Eternal youth for just $43K per day – or just exercise and eat well????
This is funny, only because for the super rich, this seems like a feasible way forward… instead of eating well and exercising. A really interesting insight into how broken our thinking on health truly is.
https://ama.com.au/ausmed/eternal-youth-may-be-yours-just-43000-day
Eternal youth may be yours, for just $43,000 a day

Like a bad fairy tale, scientists believe they have developed a way to stop people getting older, but at a cost that puts it out of the reach of all but the super-rich.
A team of researchers at the University of New South Wales, working in collaboration with geneticists at Harvard Medical School, claim to have unlocked the secret to eternal youth, and to have developed a compound they say not only halts the ageing process, but can turn back the years.
The catch is, the treatment is prohibitively expensive, with estimates it would cost the average 86 kilogram man $43,000 a day, and the average 71 kilo woman $35,500 a day.
The compound was developed based on an understanding of how and why human cells age.
A series of molecular events enable communication inside cells between the mitochondria – the energy source for cells, enabling them to carry out key biological functions – and the nucleus. The researchers found that when there is a communication breakdown between the mitochondria and the nucleus of the cell, the ageing process accelerates.
As humans age, levels of the chemical NAD (which initiates communication between the mitochondria and the nucleus), decline. Until now, the only way to arrest this process has been through calorie-restricted diets and intensive exercise.
But the researchers, led by University of New South Wales and Harvard University molecular biologist Professor David Sinclair, have developed a compound – nicotinamide mononucleotide – that, when injected, transforms into NAD, repairing broken communication networks and rapidly restoring communication and mitochondria function.
In effect, it mimics the results achieved by eating well and exercising.
“The ageing process we discovered is like a married couple. When they are young, they communicate well but, over time, living in close quarters for many years, communication breaks down,” Professor Sinclair said. “And just like a couple, restoring communication solved the problem.”
In the study, the researchers used mice considered equivalent to a 60-year-old human and found that, within a week of receiving the compound, the mice resembled a 20-year-old in some aspects including the degree of muscle wastage, insulin resistance and inflammation.
Professor Sinclair said that, if the results stand, then ageing may be a reversible condition if it is caught early.
“It may be in the future that your age in years isn’t going to matter as much as your biological age,” Professor Sinclair said.
“What we’ve shown here is that you can turn back your biological age or, at least, we think we have found a way to do that.”
The problem is, the compound is prohibitively expensive, at least at the moment.
It costs $1000 per gram to produce, and in tests so far it has been applied at a rate equivalent to 500 milligrams for every kilogram of body weight, each day.
Professor Sinclair admitted the cost was major consideration, and said the team was looking at was to produce the compound more cheaply.
As part of their research, the scientists investigated HIF-1, an intrusive molecule that foils communication but also has a role in cancer.
It has been known for some time that HIF-1 is switched on in many cancers, but the researchers found it also switches on during ageing.
“We become cancer-like in our ageing process,” Professor Sinclair said. “Nobody has linked cancer and ageing like this before, and it may explain why the greatest risk of cancer is age.”
Researchers are now looking at longer-term outcomes the NAD-producing compound has on mice, and suggest human trials may begin as early as next year.
They are exploring whether, in addition to halting ageing, the compound can be used to safely treat a range of rare mitochondrial diseases and other conditions, such as cancer, type 1 and type 2 diabetes, muscular dystrophy, other muscle-wasting conditions and inflammatory diseases.
The research was published in the journal Cell.
Kirsty Waterford
The universe is not made of atoms. It’s made of TINY STORIES.
Sir Muir Gray – ACSQHC Presentation
- We’re entering a new era in the NHS where there is “NO MORE MONEY“
@19min: describes “three big businesses in respiratory disease – asthma, COPD, apnoea”
- Value = Outcomes / Costs
- Outcome = Effectiveness (EBM+Quality) – Harm (Safety)
- Costs = Money + Time + Carbon
@22mins: moving from guideline care to personalised care
@26mins: Bureaucracy is important and necessary, but should stick to what it’s good at doing:
- The fair and open employment and promotion of people
- The un-corrupt management of money
- !! Not the curing of disease or delivery of health care – populations defined by need, not jurisdiction
@32mins: law of diminishing returns – benefits plateau as invested resources rise
@33mins: Harmful effects of healthcare increase in direct proportion to the resources invested
@34mins: combine the 2 curves – get a j-shaped curve with a point of optimality – the point of investment after which, the health gain may start to decline
@35mins: as the rate of intervention in the population increases, the balance of benefit and harm also changes for the individual patient
@37mins: value spectrum
[HIGH VALUE]
– necessary
– appropriate
[LOW VALUE]
– inappropriate
– futile
[NEGATIVE VALUE]
@39mins: The Payers’ Archipelago
20th Century Care >> 21st Century Care
Doctor >> Patient
Bureaucracy >> Network
Institutions >> Systems
@42mins: clinicians responsible for whole populations, not just the patients in front of them
@45mins: How to start a revolution
– change the culture – destabilise and constrain; control language
– engage patients and citizens, and the future leaders of 2033
– structure doesn’t matter (5%)
– systems (40%)
– culture or mindset (50%)
@46mins: Culture – the shared tacit assumptions of a group that it has learned in coping with external threats and dealing with internal relationships” Schein (1999) The Corporate Culture Survival Guide
@47mins50s: data doesn’t change the world, emotion changes the world
– atlases written for OMG effect
– programme budgeting
destabilise then constrain then change the language
@49mins: MUDA means waste — resource consumption that doesn’t contribute to the outcome. motonai – the feeling of regret that resources are being wasted. ban old language.
@51mins: mandatory training in new thinking
The Third Healthcare Revolution is already underway
1. PHONE
2. CITIZENS
3. KNOWLEDGE
The third healthcare revolution will come out of the barrel of a smartphone
@56mins: Healthcare is too complex to be run by bureaucracies or markets. Work like an ant colony – neither markets nor bureaucracies can solve the challenges of complexity.
PDF: Sir-Muir-Gray-Masterclass-presentation-1-Oct-2013
ASQHC Presentation link: http://www.safetyandquality.gov.au/our-work/medical-practice-variation/presentations/
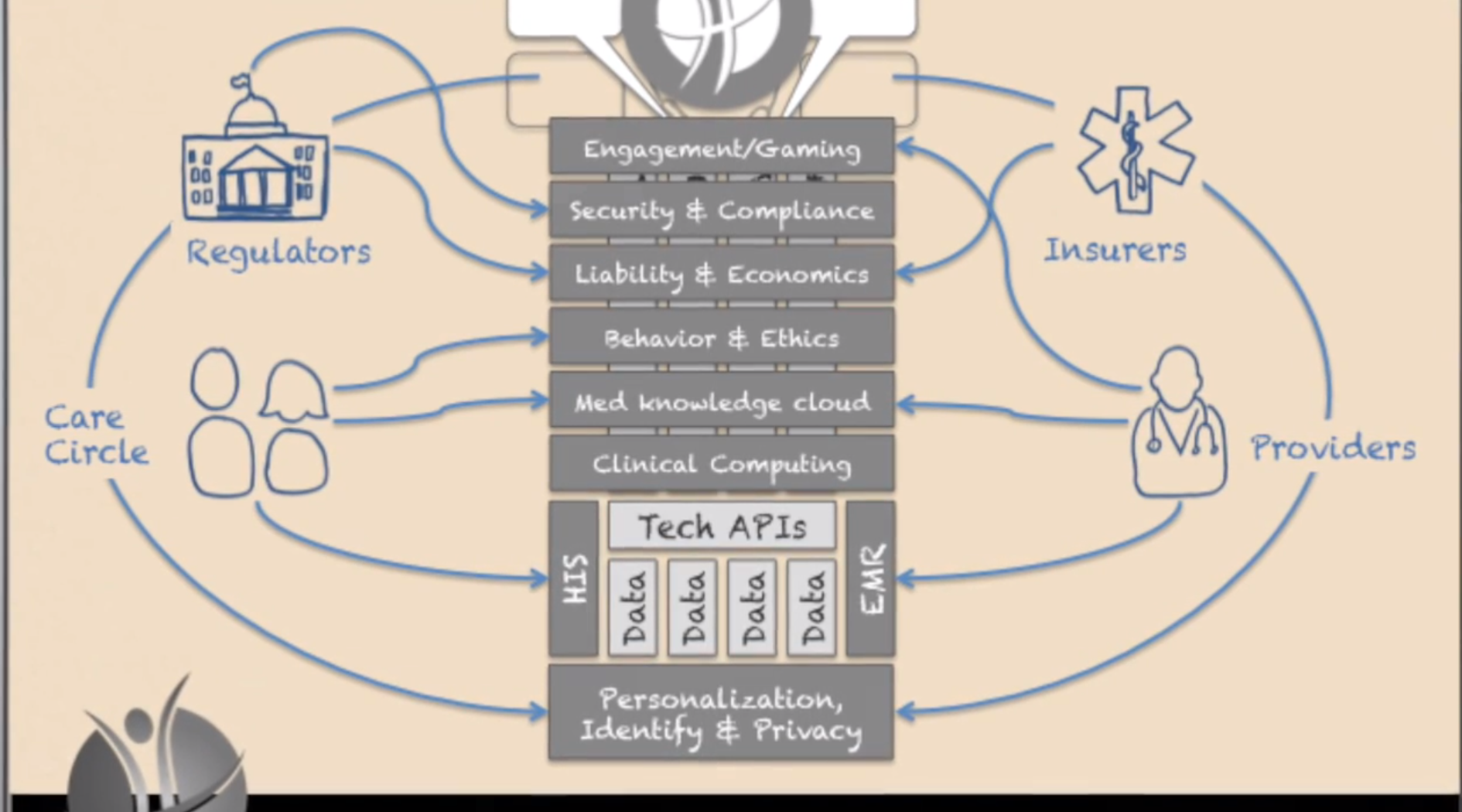
Forcing the prevention industry – a 10 year journey
Vision
- The Future of Human API www.thehumanapi.com
- Forcing the prevention industry into existence
- Stage Zero disease detection and treatment
Critical trends:
- lab-in-a-box diagnostics
- quantified self
- medical printing
When these trends converge, there’ll be an inflection point where a market is established.
Health data moves from system of record >> system of engagement.
Promoting the evolution from a Product mentality to a Market mentality
As treatment starts to focus on Stage Zero/pre-clinical disease, it turns into prevention.
Video: http://www.youtube.com/watch?feature=player_embedded&v=gJHaoqeucX8
The Asymptotic Shift From Disease To Prevention–Thoughts For Digital Health
I’ve stolen from two great thinkers, so let’s get that out of the way. The first isDaniel Kraft, MD. Daniel Kraft is a Stanford and Harvard trained physician-scientist, inventor, entrepreneur, and innovator. He’s the founded and Executive Director of FutureMed, a program that explores convergent, rapidly developing technologies and their potential in biomedicine and healthcare. He’s also a go-to source on digital health. I’m stealing “zero stage disease” from Dr. Kraft. Simply put, it’s the concept of disease at its most early, sub-clinical stage. It’s a point where interventions can halt or change a process and potentially eliminate any significant manifestation of disease.
The second source of inspiration is Richie Etwaru. He is a brilliant and compelling speaker and a champion for global innovation, Mr. Etwaru, is responsible for defining and delivering the global next generation enterprise product suite for health and life sciences at Cegedim RelationshipManagement. His inspiring video, The Future of Human API really got me thinking.
At the heart of Mr. Etwaru’s discussion is the emergence of prevention–not treatment–as the “next big thing”.
Ok, nothing new so far. But the important changes seen in the digital health movement have given us a profound opportunity to move away from the conventional clinical identification of a that golf-ball sized tumor in your chest to a much more sophisticated and subtle observation. We are beginning to find a new disease stage–different from the numbers and letters seen in cancer staging. The disease stage is getting closer and closer to zero. It’s taking an asymptotic path that connects disease with prevention. The point here is that the holy grail of prevention isn’t born of health and wellness. Prevention is born out of disease and our new-found ability to find it by looking closer and earlier. Think quantified self and Google Calico.
And here lies the magic.
We all live in the era of disease. And the vast majority of healthcare costs are spent after something happens. The simple reality is that prevention is difficult to fund and the health-economic model is so skewed to sickness and the end of life that it’s almost impossible to change. But if we can treat illness earlier and earlier–the concept of an asymptote–we build a model where prevention and disease share the very same border. They become, in essence, the same. And it’s here that early, early, early disease stage recognition (Stage Zero) becomes prevention. The combination of passive (sensor mediated) observation and proactive life-style strategies for disease suppression can define a new era of health and wellness.
Keep Critical! Follow me on Twitter and stay healthy!




David L. Katz, MD, MPH
January 21, 2014